Keywords
1. Chondrocyte autophagy
2. ER stress and cell survival
3. PERK signaling pathway
4. ATG5 and ATG7 in cell homeostasis
5. Autophagy enhancement therapy
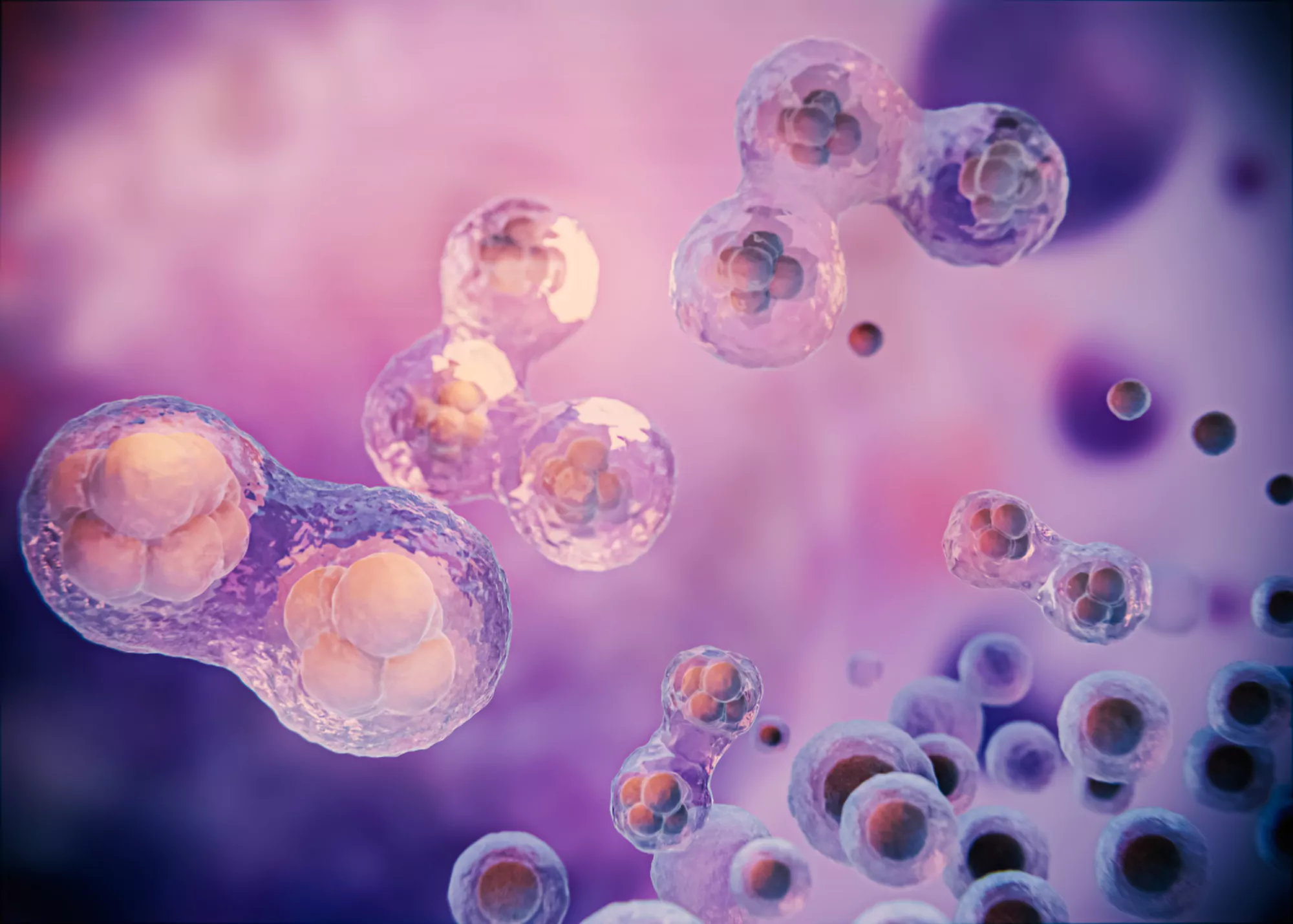
The study of cellular mechanisms underlying health and disease has always garnered significant attention for its potential therapeutic applications. In recent years, an intricate dance between autophagy and endoplasmic reticulum (ER) stress has taken center stage, capturing the interest of cell biologists and clinicians alike. At the heart of this dynamic interplay is the unfolded protein response (UPR) pathway, through which cells respond to ER stress.
A breakthrough study by Zheng Wei, Xie Weiwei, Yin Danyang, Luo Rui, Liu Min, and Guo Fengjin, published in Cell Communication and Signaling, has cast light on this complex relationship by elucidating the role of autophagy-related genes ATG5 and ATG7 in chondrocytes, the cells essential to cartilage health.
DOI: 10.1186/s12964-019-0353-3
The research emerges on the backdrop of autophagy’s well-established role in controlling cellular stress outcomes by degrading damaged cell organelles and misfolded proteins — a process termed “cellular housekeeping.” In a specific form known as ER-phagy, autophagy is specialised for the degradation of the endoplasmic reticulum, thus ensuring protein balance within the cell.
Central to the findings of the study are two key autophagy genes: ATG5 and ATG7. Extensive analyses, leveraging a range of advanced techniques from immunoblotting and RT-PCR to flow cytometry and transmission electron microscopy, were conducted to build a comprehensive picture of the effects that the expression of these genes has on various cellular processes.
The researchers’ pursuit to understand the consequences of ATG5 and ATG7 overexpression has produced compelling insights. When faced with stressed environments induced by treatment with Tunicamycin (Tm), an ER stress activator, cells kick-started autophagy to mitigate the potential damage. Conversely, when autophagy was stimulated by treatments such as Rapamycin, an astonishing observation came to light: autophagy, in turn, inhibited ER stress.
Diving deeper, the study discovered that overexpressing ATG5 or ATG7 not only promoted autophagic activity but also individually curtailed ER stress. A combined overexpression of both genes led to an even more pronounced effect, enhancing cell survivability amid stressful conditions.
The plot thickened when it came to the role of these genes in cell proliferation and death. Whether it was ATG5, ATG7, or both acting together, chondrocyte populations declined less and migrated more into the S phase of the cell cycle, an indication of increased proliferation. This outcome underscores a decreased rate of apoptosis, hinting at the protective effects these genes hold against cell death.
One cannot discuss autophagy and ER stress without acknowledging their relationship with the PERK signaling pathway, a vital branch of the UPR that performs a tightrope act between survival and apoptosis. The collaborative mechanisms of PERK signaling and ATG5/7 expression are akin to a precisely tuned symphony, balancing the scales of cellular fate.
The synergistic effects of small interfering RNAs targeting PERK and Nrf2 versus the antagonistic interactions with ATF4 interception further validated the central role of PERK signaling not only in autophagy and ER stress responses but also in the essential process of ER-phagy.
With the increasing prevalence of joint-related pathologies such as osteoarthritis, the understanding of chondrocyte survivability and the maintenance of healthy cartilage tissue is of undeniable importance. Knowing that autophagy stands as a protective mechanism against ER stress-induced apoptotic cell death, granting cells a lifeline in a time of crisis, the findings of this study carry immense potential for clinical translation.
The protective alliance between ATG5/7 and PERK signaling in chondrocytes opens avenues for developing autophagy enhancement therapies or agents targeting the PERK pathway. Such interventions could be revolutionary in treating degenerative diseases characterized by increased cell stress and impaired autophagy, including various forms of arthritis.
In conclusion, the remarkable study by Zheng Wei and colleagues delves beyond the surface-level understanding of autophagy and ER stress, tracing the intricate lines that connect cellular survival, apoptosis, and proliferation. Their discoveries not only contribute extensively to the cell biology literature but also set the stage for future research that may eventually lead to breakthroughs in therapies for joint degeneration and perhaps beyond.
As the authors look forward to the ramifications of their work, it is worth noting the vast expanse of unknowns that still lies ahead. While the precise mechanisms through which autophagy genes orchestrate their protective roles remain to be fully deciphered, the powerful influence of ATG5 and ATG7 on chondrocyte fate under stress is unmistakable.
References
1. Amber, N. H., Dan, J. L., Thomas, R. G., & Edmund, B. R. (2013). Autophagy: regulation and role in development. Autophagy, 9(7), 951–972. doi: 10.4161/auto.24273.
2. Chun, Y., & Kim, J. (2018). Autophagy: an essential degradation program for cellular homeostasis and life. Cells, 7(12), 278. doi: 10.3390/cells7120278.
3. White, E., Mehnert, J. M., & Chan, C. S. (2015). Autophagy, metabolism, and Cancer. Clin Cancer Res, 21(22), 5037–5046. doi: 10.1158/1078-0432.CCR-15-0490.
4. Mathiassen, S. G., De Zio, D., & Cecconi, F. (2017). Autophagy and the cell cycle: a complex landscape. Frontiers in Oncology, 7, 51. doi: 10.3389/fonc.2017.00051.
5. Rubinsztein, D. C., Gestwicki, J. E., Murphy, L. O., & Klionsky, D. J. (2007). Potential therapeutic applications of autophagy. Nature Reviews Drug Discovery, 6, 304–312. doi: 10.1038/nrd2272.