Keywords
1. Diverting Ostomy
2. Ileostomy
3. Colostomy
4. Colorectal Surgery
5. Anastomotic Leakage
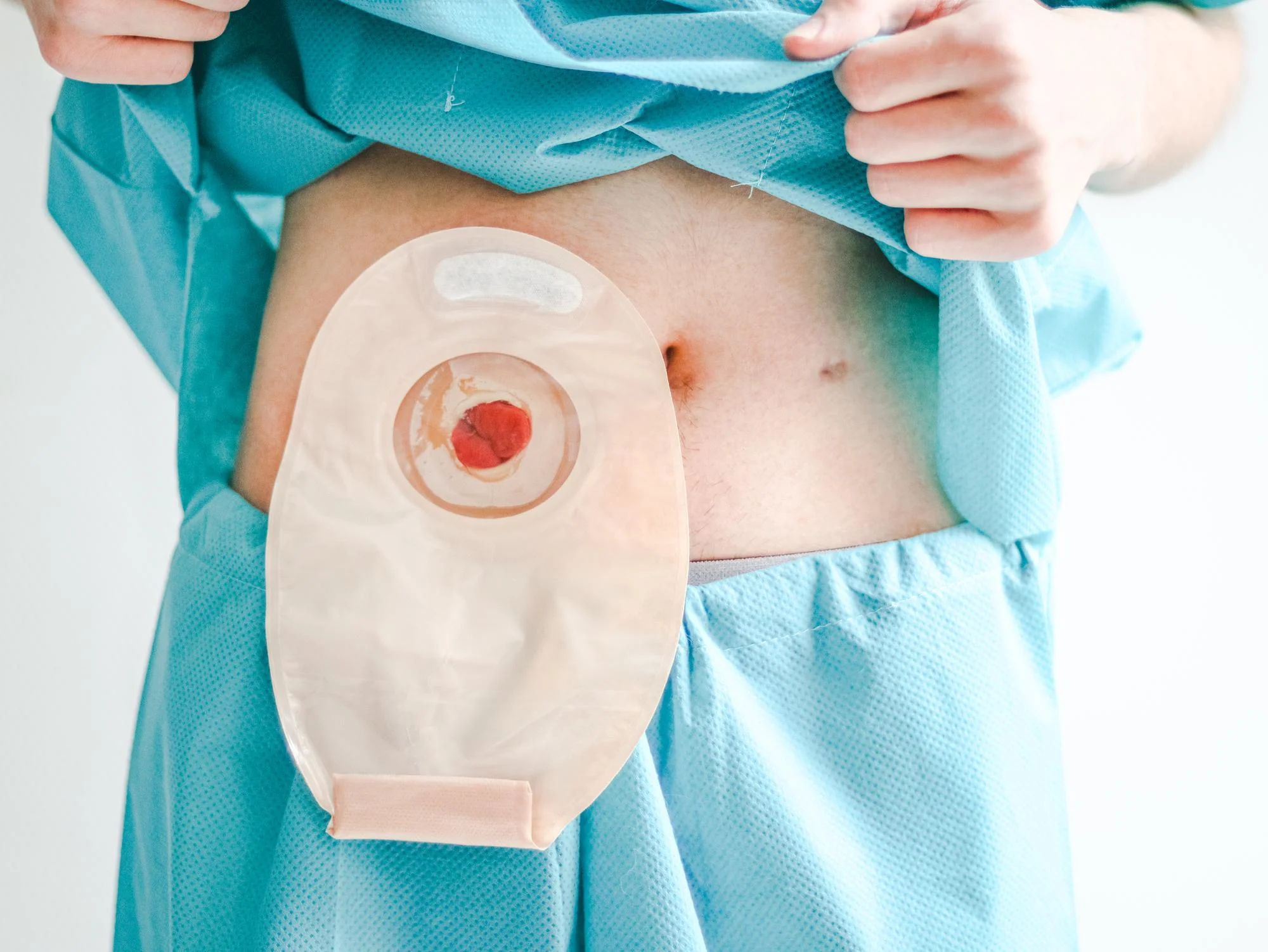
In the realm of colorectal surgery, creating a diverting ostomy is a pivotal measure in the management of various colorectal conditions. With a history embedded in helping to heal and protect surgical interventions, the decision to use fecal diversion stands at the forefront of preoperative planning. An extensive review of current literature by Plasencia Alexis A. and Bahna Heidi H., through their article titled “Diverting Ostomy: For Whom, When, What, Where, and Why,” published in the “Clinics in Colon and Rectal Surgery” journal, sheds light on the nuanced clinical scenarios where a diverting stoma is most appropriately applied.
The article, with DOI 10.1055/s-0038-1677004, provides insights into the various justifications for diverting ostomy. These range from its utilization in protecting low pelvic anastomoses from stress resulting from fecal passages to its role in managing complex inflammatory bowel disease, diverticular disease, and obstructing colorectal cancers.
For instance, diverting loop ileostomy is preferred over loop colostomy. This preference is substantiated by pertinent literature, including a seminal meta-analysis by Geng et al. (2015), which weighs the surgical complications related to these interventions (PMC5210131). The rationale behind this preference lies in several factors, including a decrease in irritation and complication rates with ileostomies as demonstrated by Rondelli et al. (2009), who found a decreased incidence of postoperative complications for ileostomies in their comprehensive meta-analysis (Int J Colorectal Dis, 19219439).
This distinction is further underscored by Klink et al. (2011), who showed that there’s a lesser risk of dehydration and subsequent readmission with ileostomies compared to colostomies (Int J Colorectal Dis, 21221605). When it comes to fecal diversion for low pelvic anastomoses, which are significantly vulnerable to dehiscence, the literature demonstrates that ileostomies can markedly decrease the clinical impact of potential leaks, a finding supported by Ihnát et al. (2016) in their assessment of the protective benefits of ileostomies (Surg Endosc, 26902615).
As for the high-risk scenario of diverticular perforation, the practice of primary anastomosis followed by a diverting ileostomy has been regarded as safe. This assertion is further strengthened by the trials analyzed by Mrak et al. (2016), revealing that fecal diversion in these cases not only reduces morbidity but can also be reversed with fewer complications than previously thought (Surgery, 26706610).
Perianal Crohn’s disease is another context where diversion plays an essential role. The severe inflammatory process often necessitates diversion to control local sepsis and foster healing, as illustrated in works by Yamamoto et al. (2000), Mueller et al. (2007), and Hong et al. (2011)—who all describe instances where fecal diversion resulted in an improvement of complex perianal disease (Br J Surg, 9529492; J Gastrointest Surg, 17436140; Colorectal Dis, 19863597).
In the case of obstructing colorectal cancer, the authors of the reviewed article posit that a diverting stoma can effectively act as a bridge to surgery. This affords patients the chance for a more stable health status preoperatively, ultimately leading to safer primary resection operations. Nurkin et al. (2013) found that the use of a proximal stoma can indeed reduce anastomotic leakage rates in patients undergoing resection for rectal cancer without substantially increasing stoma complications (Colorectal Dis, 23586660).
Challenges certainly exist in the postoperative course of ostomy formation, as evidenced by the significant morbidity surrounding the reversal of ileostomies, as well as the development of high-output stoma. In a systematic review by Chow et al. (2009), it was found that reversal procedures hold a significant morbidity rate, reiterating the need for careful patient selection and perioperative care (Int J Colorectal Dis, 19221766). Additionally, understanding the causes and management of high-output stoma, as discussed by Baker et al. (2011), is instrumental in preventing associated complications such as dehydration and renal dysfunction (Colorectal Dis, 19888956).
Despite the benefits, the literature also highlights critical considerations for ostomy creation. The risk factors for anastomotic leakage, including patient factors and surgical technique, are extensively reviewed by Rullier et al. (1998), who emphasized the importance of meticulous surgical planning and patient optimization to minimize risks (Br J Surg, 9529492).
As we look forward, it becomes increasingly clear that the evolution of fecal diversion procedures, their indications, and technical refinements must continue to adapt to the ever-changing landscape of colorectal surgical practices. The referenced article serves as a comprehensive examination of the current state of knowledge regarding this subject and calls for a continual reappraisal of guidelines to suit patient-oriented goals.
In closing, diverting ostomy remains a potent tool, with its judicious application stemming from an understanding of its benefits and potential downfalls. The meticulous body of work by Plasencia Alexis A. and Bahna Heidi H. provides an invaluable contribution to guiding surgeons in optimizing patient outcomes in this complex surgical facet.
References
1. Geng H, Z., Nasier D., Liu B., Gao H., Xu Y. K. (2015). Meta-analysis of elective surgical complications related to defunctioning loop ileostomy compared with loop colostomy after low anterior resection for rectal carcinoma. Ann R Coll Surg Engl. 97(07):494–501. DOI:10.1308/rcsann.2015.0026. PMC5210131
2. Rondelli F., Reboldi P., Rulli A., et al. (2009). Loop ileostomy versus loop colostomy for fecal diversion after colorectal or coloanal anastomosis: a meta-analysis. Int J Colorectal Dis. 24(05):479–488. DOI:10.1007/s00384-009-0663-x
3. Klink C. D., Lioupis K., Binnebösel M., et al. (2011). Diversion stoma after colorectal surgery: loop colostomy or ileostomy? Int J Colorectal Dis. 26(04):431–436. DOI:10.1007/s00384-010-1101-6
4. Ihnát P., Guňková P., Peteja M., Vávra P., Pelikán A., Zonča P. (2016). Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc. 30(11):4809–4816. DOI:10.1007/s00464-016-4796-9
5. Mrak K., Uranitsch S., Pedross F., et al. (2016). Diverting ileostomy versus no diversion after low anterior resection for rectal cancer: a prospective, randomized, multicenter trial. Surgery. 159(04):1129–1139. DOI:10.1016/j.surg.2015.11.024