Keywords
1. Hepatic Encephalopathy
2. Glymphatic System Impairment
3. Pathogenesis of Hepatic Encephalopathy
4. Hydrodynamic Hypothesis
5. Brain-Liver Connection
Introduction
Hepatic Encephalopathy (HE) is a complex neurological disorder that commonly arises in individuals with severe liver disease. It leads to a spectrum of cognitive alterations, potentially progressing to coma and death. The symptoms of HE are thought to originate from the liver’s reduced capability to detoxify harmful substances, such as ammonia, that subsequently accumulate in the blood and impair brain function. Yet, the precise mechanisms underlying the development of HE remain only partially understood. Expanding understanding of the pathophysiological processes involved in HE is crucial for the development of targeted treatments and improved patient outcomes.
A groundbreaking study published in the ‘Journal of Hepatology’ in July 2019 has challenged conventional thinking regarding hepatic encephalopathy’s development. Authored by Pasquale Gallina (Department of NEUROFARBA, Neurosurgical Unit, University of Florence, Italy) and collaborators, including Oreste Gallo, Claudio Nicoletti, and Roberto Giulio Romanelli, the study introduces a “hydrodynamic hypothesis” implicating the impairment of the glymphatic system in the pathogenesis of HE. The glymphatic system is a network involved in waste clearance from the brain, and its dysfunction might be a contributing factor to the cognitive dysfunctions observed in HE patients.
The Hydrodynamic Hypothesis
The main argument of Gallina and colleagues focuses on the similarities between the mechanisms that regulate the flow within the hepatic and glymphatic systems. The liver is known for its high vascular compliance, which allows it to accommodate significant changes in blood volume without substantial changes in pressure. This capacity is vital for its role as a detoxifying organ. Extrapolating from this, the authors propose that the glymphatic system, which relies on cerebrospinal fluid (CSF) dynamics, might exhibit similar functional properties.
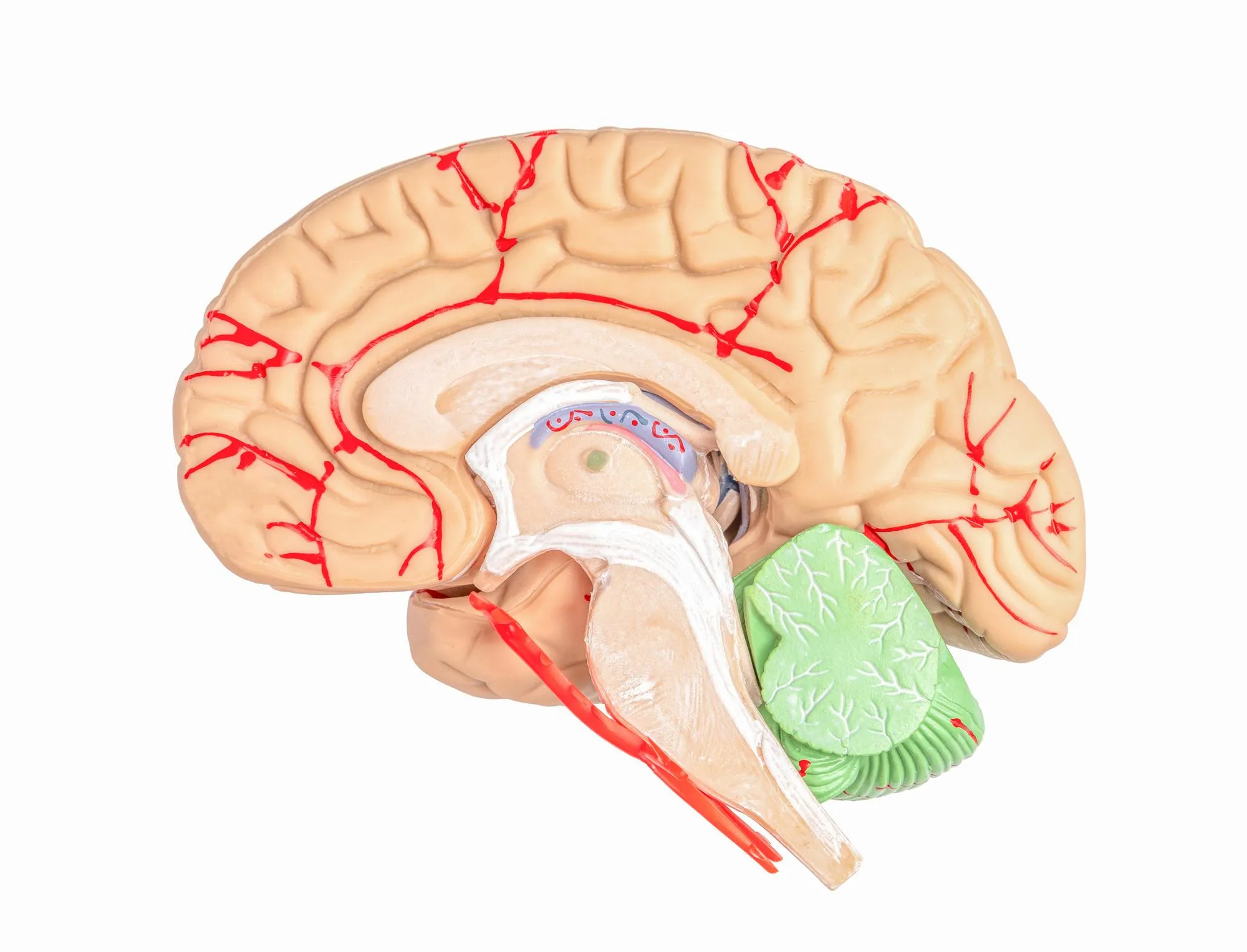
In a healthy brain, the glymphatic system facilitates the clearance of waste by using CSF to flush out potentially harmful agents from the parenchyma—brain tissue—to the perivenous spaces, where they are eventually drained into the systemic circulation. This process is believed to be driven predominantly by the pulsatility of cerebral blood flow. However, during hepatic dysfunction, the altered synthesis of liver-derived plasma proteins can affect the oncotic pressure, ultimately influencing CSF dynamics and the efficiency of the glymphatic system.
The research letter posits that HE could be a manifestation of the inhibited function of this vital clearance system, leading to the accumulation of neurotoxins and thereby cognitive dysfunction. Consequently, HE might not solely be a result of direct neurotoxicity but also a secondary consequence of impaired brain detoxification mechanisms.
Clinical Implications
This innovative hypothesis carries significant implications for the clinical management and therapeutic strategy of hepatic encephalopathy. If the impairment of the glymphatic system is a major contributor to the progression of HE, then treatments targeting the improvement of glymphatic clearance could become a crucial addition to the HE management protocol.
Indeed, the advancement of neuroimaging techniques and biomarker analysis could soon enable clinicians to monitor glymphatic function in real time, offering a more nuanced approach to the assessment of disease severity and progression. This will undoubtedly aid in tailoring interventions that don’t just address the symptoms but also tackle the underlying pathophysiological disturbances.
The study also emphasizes the importance of understanding brain-liver interaction and highlights the possibility that HE might be an early indicator of a dysfunctional liver-glymphatic axis, potentially serving as a prognostic marker for the severity of liver disease.
Future Directions
This research opens the door to an array of questions and possibilities that demand investigation. For instance, what are the molecular indicators of glymphatic system dysfunction in the context of hepatic disease? Could specific therapeutic agents help to restore or enhance glymphatic clearance? Further experimental studies and clinical trials will be needed to explore these questions and to validate the hydrodynamic hypothesis.
One promising avenue of exploration is the potential role of sleep in managing HE, as the glymphatic system is thought to be more active during sleep. Enhancing sleep quality could become an adjunct therapy in improving glymphatic circulation, thus ameliorating the cognitive symptoms of HE.
Conclusion
The hydrodynamic hypothesis for the pathogenesis of glymphatic system impairment in hepatic encephalopathy represents an innovative step forward in understanding this debilitating condition. It bridges the gap between neurology and hepatology, emphasizing the intricate connections between liver function and brain health. Though still in its theoretical phase, this model promises to reframe our approach to diagnosing, monitoring, and treating hepatic encephalopathy, potentially benefiting countless individuals affected by chronic liver diseases.
DOI: 10.1016/j.jhep.2019.02.010
References
1. Gallina, P., Gallo, O., Nicoletti, C., & Romanelli, R. G. (2019). A hydrodynamic hypothesis for the pathogenesis of glymphatic system impairment in hepatic encephalopathy. Journal of Hepatology, 71(1), 228-229.
2. Jessen, N. A., Munk, A. S., Lundgaard, I., & Nedergaard, M. (2015). The Glymphatic System: A Beginner’s Guide. Neurochemical Research, 40(12), 2583-2599.
3. Montagne, A., Barnes, S. R., Sweeney, M. D., Halliday, M. R., Sagare, A. P., Zhao, Z., … & Zlokovic, B. V. (2015). Blood-brain barrier breakdown in the aging human hippocampus. Neuron, 85(2), 296-302.
4. Rangroo Thrane, V., Thrane, A. S., Plog, B. A., Thiyagarajan, M., Iliff, J. J., Deane, R., … & Nedergaard, M. (2013). Paravascular microcirculation facilitates rapid lipid transport and astrocyte signaling in the brain. Scientific Reports, 3, 2582.
5. Rangroo Thrane, V., & Nedergaard, M. (2017). The glymphatic pathway in neurological disorders. The Lancet Neurology, 16(11), 842-852.