A recent case study reported in the “Rinsho shinkeigaku = Clinical neurology” journal, dated May 28, 2019, has highlighted an extraordinarily rare medical occurrence. A 52-year-old man presented with two instances of bacterial meningitis within a span of just six months. The peculiar aspect of this case lies in the underlying cause— a chordoma presenting as recurrent bacterial meningitis, associated with cerebrospinal fluid (CSF) leakage. The case opens discourse on a critical intersection between oncology and infectious disease, raising awareness on the importance of thorough diagnostic procedures.
Recurrence of Bacterial Meningitis Linked to Chordoma
The patient, whose case has been documented under the Digital Object Identifier (DOI) 10.5692/clinicalneurol.cn-001272, was admitted to the Nagaoka Red Cross Hospital with signs consistent with bacterial meningitis. The CSF analysis showed an increased number of neutrophils, high protein levels, and low glucose levels, known as hypoglycorrhachia. However, the surprising element was that despite these marked changes, the inflammatory reaction was found to be rather mild, and both blood and CSF cultures remained negative for bacteria.
What eventually led to the diagnosis was the observation of intermittent watery nasal discharge indicative of CSF rhinorrhea—a condition in which CSF leaks through the nose. This was a telltale sign pointing towards cerebrospinal fluid leakage, a complication often overlooked but potentially deadly due to the risk of recurrent infections.
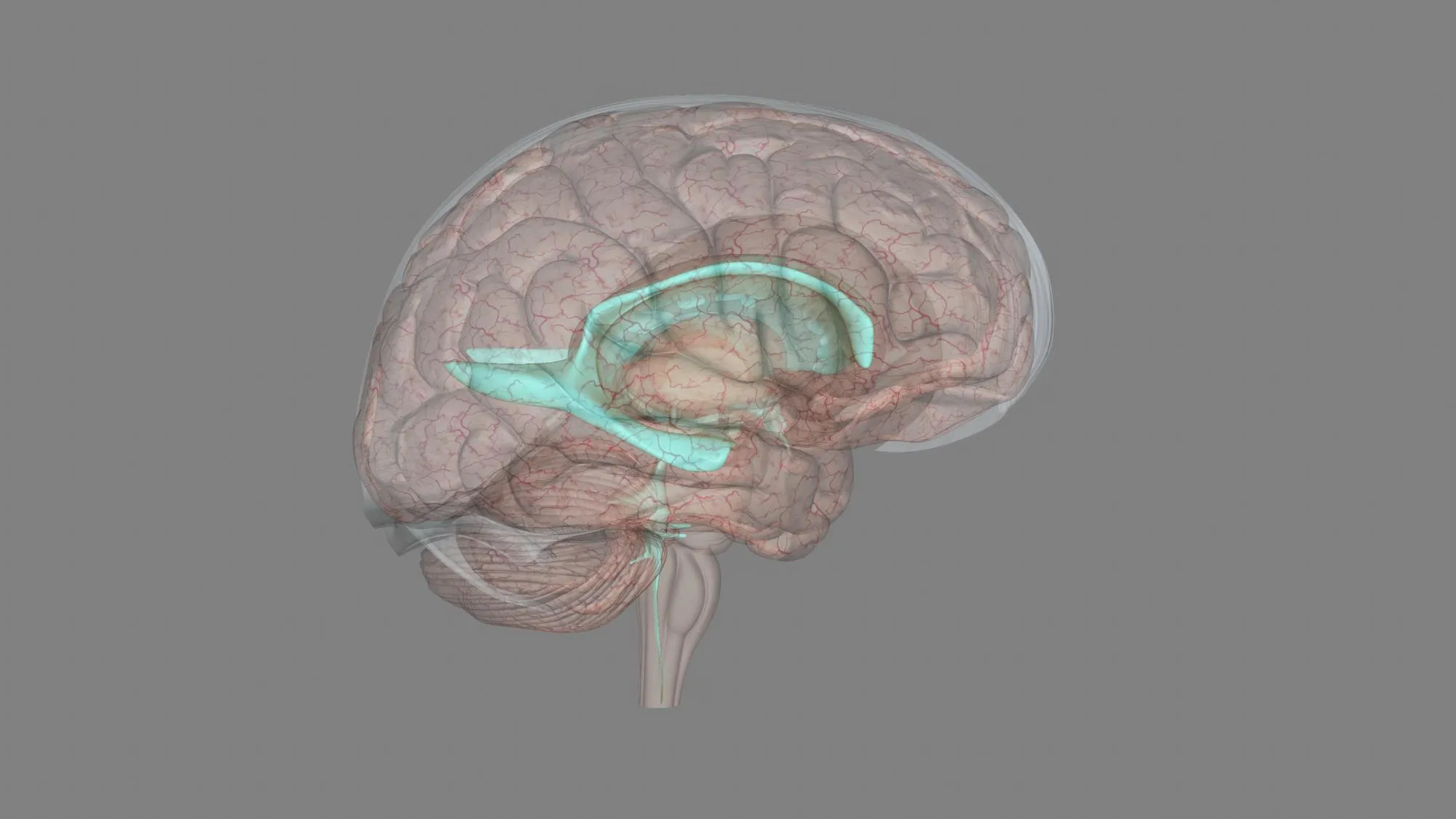
Diagnostic Imaging Reveals Underlying Cause
Diagnostic imaging was pivotal in identifying the exact cause of the recorded symptoms. Computerized tomography (CT) and magnetic resonance (MR) imaging revealed a small defect in the clival bone. This defect provided a pathway for the CSF to leak and subsequently become an entry point for pathogens leading to repeated infections. It is within this investigative context that the chordoma—a rare type of bone cancer—was diagnosed. The endoscopic transnasal repair was performed successfully, addressing the CSF leakage.
The chordoma was further confirmed pathologically through immunohistochemical staining for brachyury, a specific marker that is typically present in chordomas. The particularities of this case, captured in this report by Ando Shoichiro S and colleagues from the Department of Neurology and Pathology at Nagaoka Red Cross Hospital, reveal the complexity behind what appeared to be recurrent meningitis.
Implications for Clinical Practice
This astonishing case broadens the scope of clinical suspicion in the recurring instances of meningitis where conventional biomarkers fail to reveal the infection source. It underlines the necessity of detailed patient history-taking, particularly inquiring about symptoms indicative of CSF rhinorrhea.
The occurrence of a chordoma presenting as recurrent bacterial meningitis with CSF leakage is rare, to the point of being nearly unheard of in general clinical practice. However, this case emphasizes the need for healthcare professionals to be aware of such possibilities. It also exhibits the fundamental role that imaging techniques such as CT, MR, and MR cisternography play in unlatching the causes of cryptogenic infections.
References to contextualize the reported case can be found in a variety of sources highlighting CSF rhinorrhea, chordoma pathology, diagnostic imaging, and the complications that can arise from these conditions, emphasizing the significance of the interdisciplinary approach which was successful in this particular case.
Keywords
1. Recurrent bacterial meningitis
2. CSF rhinorrhea diagnosis
3. Chordoma symptoms
4. Cerebrospinal fluid leaks
5. Clival bone defect imaging
In conclusion, the report serves not only as a rich source of clinical knowledge and a reminder of the complexity of diagnosing rare pathologies but also stands as a testament to the diligence and acuity required in medical practice. The successful identification and treatment of the chordoma in this patient provide a notable instance of clinical acumen, underscoring the importance of a detailed and patient-centric diagnostic process.
References
1. Ando Shoichiro S, Usuda Hiroyuki H, Umeda Yoshitaka Y, Umeda Maiko M, Oyake Mutsuo M, Fujita Nobuya N. (2019). [A case of chordoma presenting as recurrent bacterial meningitis with cerebrospinal fluid leakage]. Rinsho Shinkeigaku [Clinical Neurology], 59(5), 264-267. DOI: 10.5692/clinicalneurol.cn-001272.
2. Walcott, B. P., Nahed, B. V., Mohyeldin, A., Coumans, J. V., Kahle, K. T., & Ferreira, M. J. (2012). Chordoma: current concepts, management, and future directions. Lancet Oncology, 13(2), e69-e76. DOI:10.1016/S1470-2045(11)70337-0.
3. Mazzatenta, D., Zoli, M., & Longatti, P. (2015). Cerebrospinal fluid leaks and encephaloceles: an overview. Neurosurgery Clinics of North America, 26(4), 501-509. DOI:10.1016/j.nec.2015.06.003.
4. Flanagan, A. M., Tinkler, S. M. B., Horton, M. A., Williams, D. M., & Teale, J. D. (1996). The Multinucleated Cells in Giant Cell Granulomas of the Jaw are Osteoclasts. Cancer, 77(2), 396-401. DOI:10.1002/(SICI)1097-0142(19960115)77:2<396::AID-CNCR23>3.0.CO;2-L.
5. Schisano, G., Franco, A., Nina, P., & Modugno, V. C. (1991). Nasal cerebrospinal fluid leak: diagnosis and management. Neurosurgical Review, 14(4), 289-293. DOI:10.1007/BF00320681.