Keywords
1. Cefoxitin Nebulization
2. Mycobacterium abscessus Treatment
3. Pharmacokinetics of Cefoxitin
4. Nebulized Antibiotics
5. Pulmonary Mycobacterial Infections
A recent study published in the Antimicrobial Agents and Chemotherapy journal by Mehta et al. has revealed promising preclinical data that cefoxitin, administered via nebulization, shows potential as an effective treatment for infections caused by Mycobacterium abscessus (M. abscessus). This groundbreaking research taps into the urgent need for new therapeutic strategies against this refractory pathogen, known for its formidable resistance to conventional antibiotics.
Background on Mycobacterium abscessus
Mycobacterium abscessus is a rapidly growing, multidrug-resistant non-tuberculous mycobacterium (NTM) that poses a significant treatment challenge, especially in individuals with underlying lung conditions such as cystic fibrosis (Roux et al., 2009; Nessar et al., 2012). Its intrinsic drug resistance, coupled with biofilm-forming capacity, makes M. abscessus-related chronic pulmonary infections particularly difficult to eradicate (Jarand et al., 2011). Current treatment regimens are often complicated, involving prolonged courses of multiple antibiotics with significant side effects which, unfortunately, frequently result in treatment failure (Griffith et al., 2007; van Ingen et al., 2013).
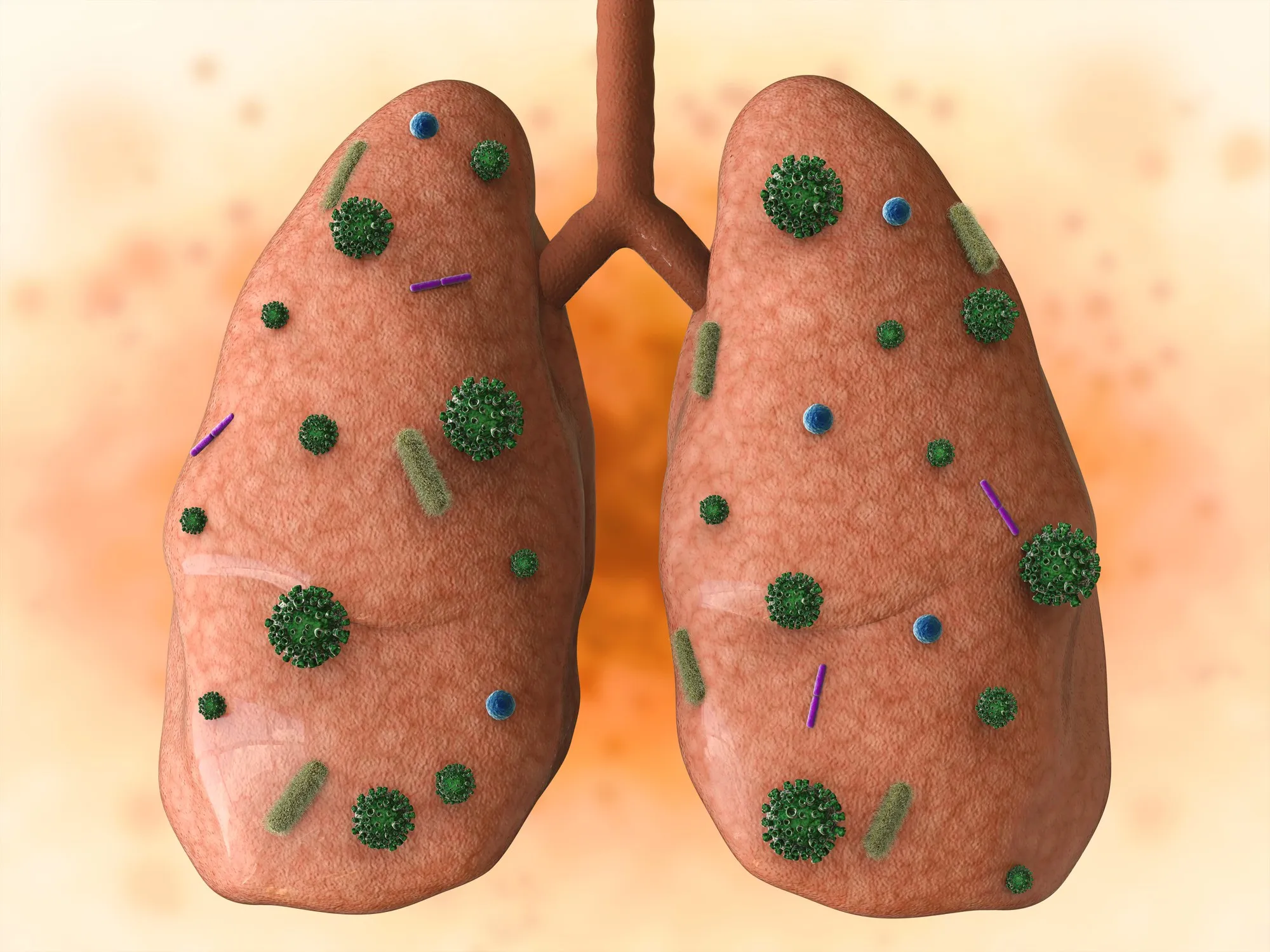
Nebulization as a Potential Route of Administration
The use of nebulized therapies is becoming increasingly prevalent in the management of pulmonary infections. Delivering medication directly into the lungs via aerosolization enhances local drug concentrations, potentially leading to improved effectiveness and reduced systemic toxicity (Flume & VanDevanter, 2015). Over recent years, nebulization has been successfully employed for antibiotics such as tobramycin and colistin in cystic fibrosis patients, providing a model for similar applications against other pulmonary pathogens (Gontijo et al., 2014; Gontijo et al., 2014; Marchand et al., 2016; Marchand et al., 2015).
The Study: Preclinical Testing of Cefoxitin Nebulization
Researchers assessed the pharmacokinetic (PK) and pharmacodynamic (PD) characteristics of cefoxitin in an animal model to determine whether sufficient drug concentrations could be achieved in the lungs through nebulization to treat M. abscessus.
The study demonstrated that nebulized cefoxitin, administered to Sprague-Dawley rats, achieved high lung tissue concentrations that surpassed the minimum inhibitory concentrations (MICs) for most strains of M. abscessus. According to Mehta et al., these findings give a clear indication of the potential for cefoxitin nebulization to provide effective treatment against M. abscessus pulmonary infections without the systemic exposure that commonly leads to adverse side effects.
The Implications and Future Directions
This preclinical investigation opens a pathway for further development of nebulized cefoxitin as a viable option for M. abscessus infections. The favorable pharmacokinetic profile of cefoxitin when delivered directly to the lungs suggests a targeted approach with potential efficacy and reduced systemic exposure as compared to traditional intravenous administration.
These findings align with recent explorations into the nebulization of other antimicrobial agents, including aminoglycosides and cephalosporins (Marchand et al., 2018; Boisson et al., 2018). Importantly, it highlights the ongoing need for continued research into novel delivery methods and agents that can overcome the resistance barrier presented by M. abscessus.
Cefoxitin, a second-generation cephalosporin, has demonstrated in vitro effectiveness against M. abscessus, holding promise for individuals suffering from this challenging infection (Lavollay et al., 2014; Ferro et al., 2015). Previous data have reported the shortcomings of the currently recommended triple therapy using amikacin, cefoxitin, and clarithromycin, necessitating the exploration of alternative delivery methods such as nebulization (Ferro et al., 2016).
Considerations for Clinical Translation
It is essential to acknowledge the leap from preclinical research to clinical application involves numerous considerations. These include the establishment of dosing regimens, the optimization of nebulizer devices, patient compliance, and the evaluation of potential risks. A thorough understanding of the balance between the PK/PD parameters and the dynamics of pulmonary M. abscessus infections will be imperative (Levison & Levison, 2009).
Moreover, the physicochemical stability of cefoxitin during nebulization, which is imperative to ensure therapeutic efficacy, will need to be thoroughly evaluated in the context of human use (Rominski et al., 2017; Schoutrop et al., 2018). Also, special attention must be paid to the pharmacokinetics within the human lung, which may significantly differ from animal models given the variations in lung anatomy and function (Zhang et al., 2008; Yapa et al., 2014).
Conclusion
As the threat of antimicrobial resistance looms large, the search for resourceful and effective treatments against tough-to-treat pathogens like M. abscessus becomes increasingly vital. The research led by Mehta and colleagues offers hope and a potential new direction in the treatment of such recalcitrant infections.
Before widespread clinical application, however, further studies, including human clinical trials, will be necessary to establish safety and efficacy. Optimal outcomes will likely require a multifaceted approach, combining advances in drug delivery technology with the ever-evolving understanding of M. abscessus pathophysiology.
The potential of nebulized cefoxitin heralds a significant step toward advancing the care of patients with M. abscessus pulmonary disease, reinforcing the value of innovative research in overcoming the challenges posed by antibiotic resistance.
References
1. Roux A-L, Catherinot E, Ripoll F, Soismier N, Macheras E, Ravilly S, Bellis G, et al. J Clin Microbiol. 2009. doi:10.1128/JCM.01257-09.
2. Nessar R, Cambau E, Reyrat JM, Murray A, Gicquel B. J Antimicrob Chemother. 2012. doi:10.1093/jac/dkr578.
3. Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL. Clin Infect Dis. 2011. doi:10.1093/cid/ciq237.
4. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. Am J Respir Crit Care Med. 2007. doi:10.1164/rccm.200604-571ST.
5. van Ingen J, Ferro BE, Hoefsloot W, Boeree MJ, van Soolingen D. Expert Rev Anti Infect Ther. 2013. doi:10.1586/14787210.2013.830413.
DOI: 10.1128/AAC.02651-18
The research article can be accessed directly here: PMC6591628