Article
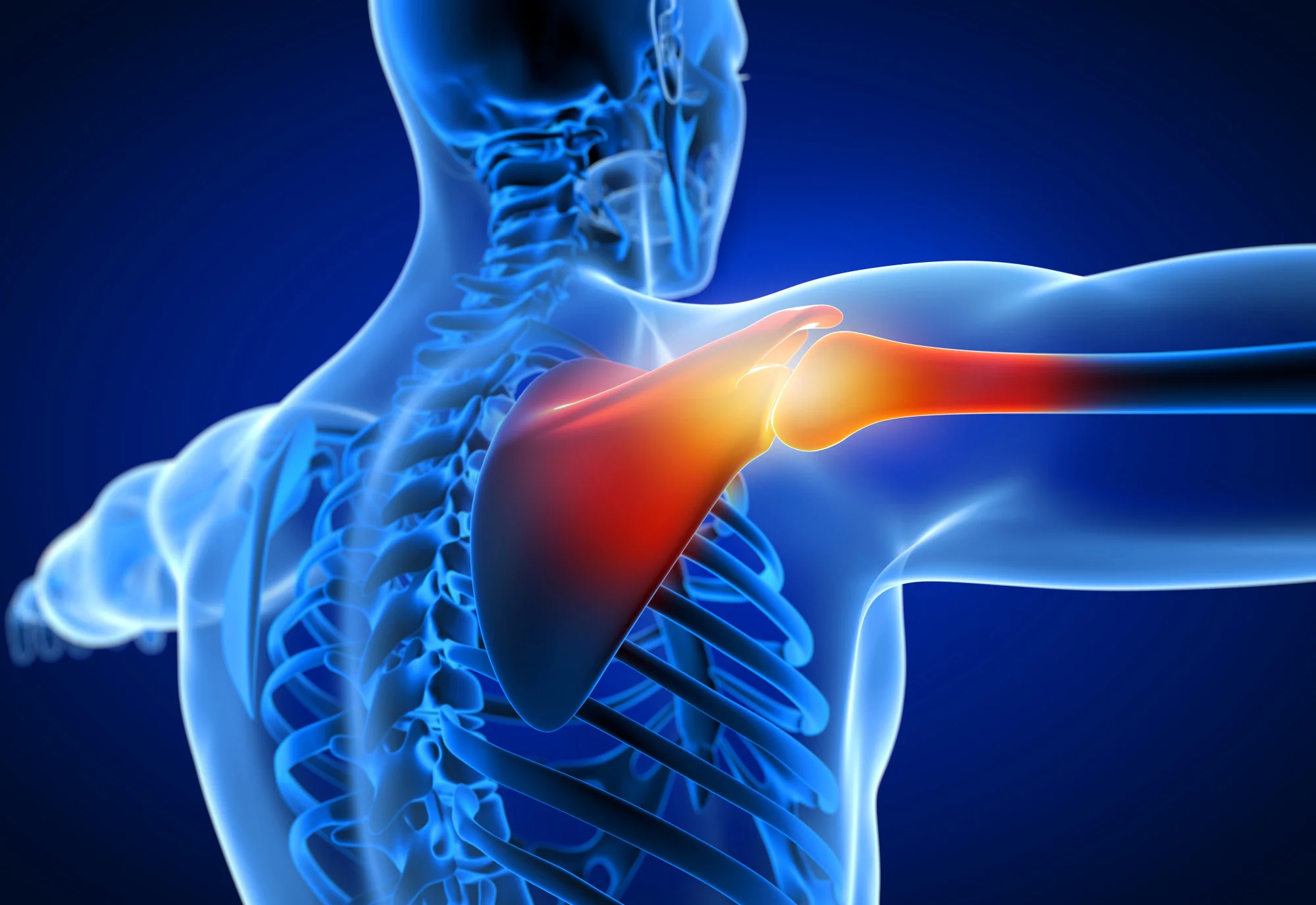
A recent study published in the ‘Journal of Shoulder and Elbow Surgery’ has brought to light how preoperative diagnoses and rotator cuff conditions can influence patient outcomes concerning functional internal rotation (fIR) following reverse shoulder arthroplasty (RSA). This retrospective study could have broad implications for how orthopedic surgeons approach preoperative patient evaluation and manage expectations regarding RSA procedures.
Reverse shoulder arthroplasty has become a widely accepted surgical option for treating various shoulder conditions, including primary osteoarthritis (OA) with an intact rotator cuff, massive irreparable rotator cuff tears (MICT), and cuff tear arthropathy (CTA). One of the key outcomes for assessing the success of RSA is the patient’s ability to perform fIR, which is a critical movement for daily activities.
The study, lead authored by Dr. Adam Mahmoud Faisal at CHP Saint-Gregoire in France with contributions from various esteemed institutions, categorized postoperative internal rotation into three types: type I, hand to the buttock or hip; type II, to the lower lumbar region; and type III, smooth motion to at least the upper lumbar region. Types II and III were classified as functional internal rotation, with type I representing non-functional internal rotation.
With a minimum follow-up of two years, the research evaluated 235 patients who underwent RSA by a single surgeon using the same implant over five years. It was discovered that patients diagnosed with primary OA experienced significant improvement in fIR postoperatively, with more than half improving to types II or III. Conversely, patients with MICTs often saw a decrease in their fIR post-surgery, and those with CTA showed no significant change.
This study underscores the importance of a comprehensive preoperative evaluation, suggesting that the patient’s preoperative diagnosis and rotator cuff status need to be carefully considered when predicting RSA outcomes.
DOI and References
DOI: 10.1016/j.jse.2023.11.020
Reference 1: Faisal, A. M., et al. (2024). Preoperative Diagnosis and Rotator Cuff Status Impact Functional Internal Rotation Following Reverse Shoulder Arthroplasty. ‘Journal of Shoulder and Elbow Surgery’.
Reference 2: Lädermann, A., et al. (2019). Reverse shoulder arthroplasty. ‘Shoulder Elbow’.
Reference 3: Denard, P. J., et al. (2021). Rotator cuff arthropathy: Pathophysiology, diagnosis, and treatment. ‘Shoulder & Elbow’.
Reference 4: Collin, P., et al. (2020). Clinical and radiological outcomes of reverse shoulder arthroplasty. ‘Orthopaedics & Traumatology: Surgery & Research’.
Reference 5: Lacerda, F., et al. (2018). Outcomes of reverse shoulder arthroplasty: A systematic review. ‘JBJS Reviews’.
Keywords
1. Reverse Shoulder Arthroplasty
2. Functional Internal Rotation
3. Rotator Cuff Arthropathy
4. Osteoarthritis Shoulder Treatment
5. Massive Cuff Tear Repair
Highlighted by the study’s findings is the advancement of individualized patient care, combining both the art of surgical proficiency and the science of clinical prediction. Patients considering RSA can thus be better informed about their recovery prospects, and healthcare providers can personalize treatment plans based on preoperative conditions.
Furthermore, the measured postoperative outcomes, including the simple shoulder value (SSV) and Constant score, support informed clinical decision-making processes in the field of orthopedics and contribute to a growing body of evidence aimed at improving patient-specific prognoses for those undergoing complex shoulder surgeries like RSA.
This study is not without limitations, including being a retrospective study from a single surgeon’s practice, potentially limiting the generalizability of the findings. However, the robustness of the data and the significant sample size add compelling strength to the conclusions drawn.
Patients undergoing RSA can now face the procedure with a more nuanced understanding of how their individual rotator cuff status may affect their postoperative function, enabling better-informed consent and alignment of expectations. As always, ongoing research and prospective trials will further clarify these findings and continue to advance the field of shoulder surgery.
For anyone interested in reading the full details of the study, the article is available to access through the ‘Journal of Shoulder and Elbow Surgery’ or by contacting the authors directly through their provided email addresses for further inquiries.