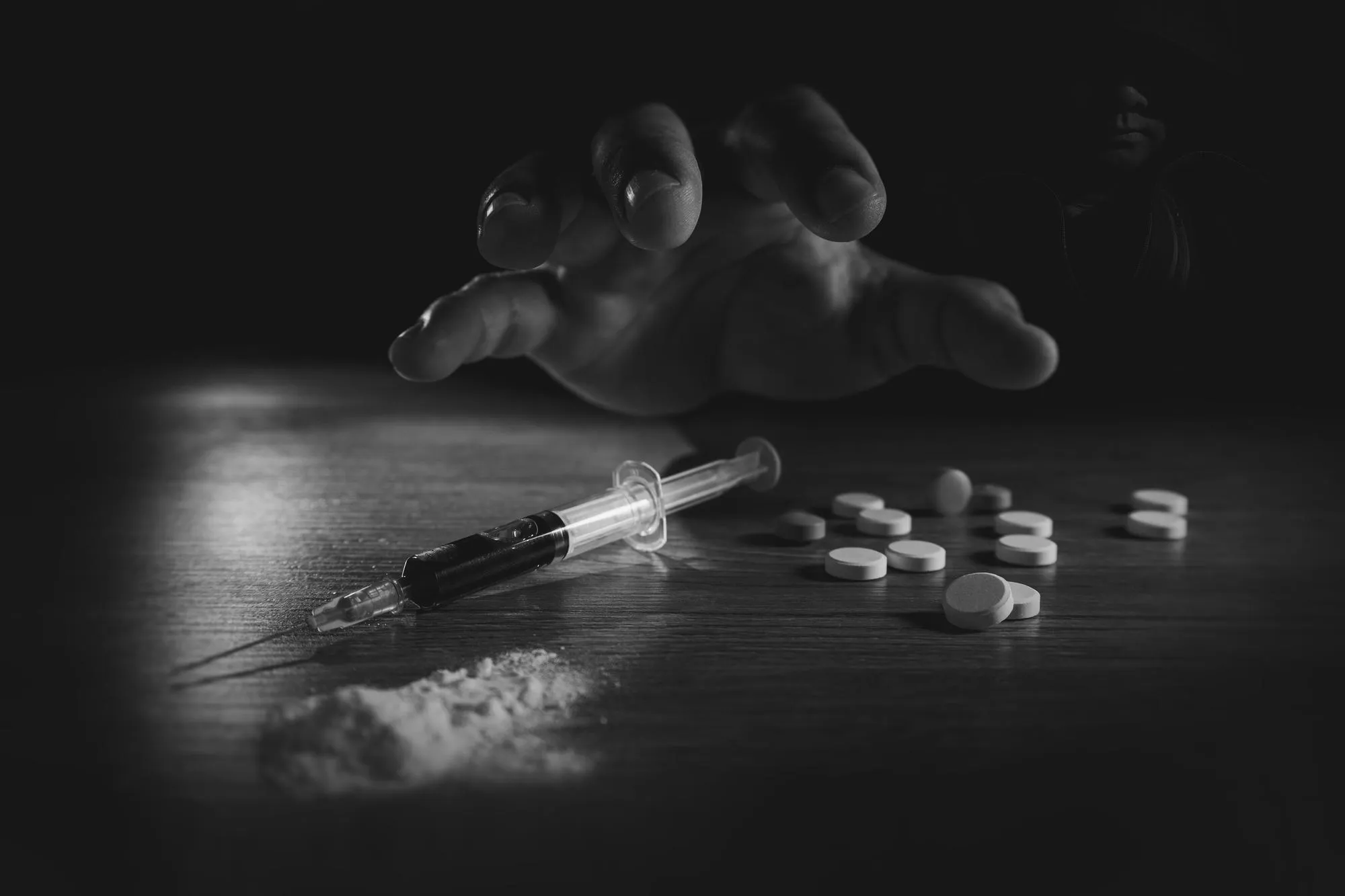
In a move to combat the opioid crisis among the homeless population, the San Francisco Street Medicine Team has implemented a pilot program that provides low barrier buprenorphine treatment to persons experiencing homelessness who inject heroin. The revealing study, published in Addiction Science & Clinical Practice, showcases both the challenges faced and progress made with this unique approach to opioid use disorder (OUD) treatment among a highly vulnerable demographic.
DOI: 10.1186/s13722-019-0149-1
The pilot program, initiated in 2016, was designed to provide easy access to care and promote sustained engagement in treatment as a means to combat opioid use and improve overall health outcomes. The study conducted a retrospective chart review spanning November 2016 to October 2017 and involved patients who received at least one buprenorphine prescription through this initiative. The results shed light on the nature of the participants involved, the retention rates over a period of 12 months, levels of opioid use, and the occurrence of adverse events such as death and nonfatal opioid overdoses.
Demographics and Comorbidities: The study analyzed data from 95 individuals with a mean age of 39.2 years, all of whom reported homelessness and injecting heroin. Notably, medical and psychiatric comorbidities as well as co-occurring substance use were prevalent among this cohort.
Treatment Retention and Opioid Use: Retention rates in the program tell a story of gradual diminution over time, with 63% retained at one month and only 26% at 12 months. Similar trends were observed for retention on buprenorphine, with 37% at one month decreasing to 18% at 12 months. Moreover, 23% of patients had at least one opioid-negative, buprenorphine-positive urine toxicology test, suggesting some level of success in reducing illicit opioid use among participants.
Adverse Events: Over the observation period, one fatal overdose due to fentanyl was reported, alongside four patients presenting on six occasions with non-fatal overdoses requiring the administration of naloxone.
The study exposes the complex realities of OUD treatment in homeless populations yet reflects a measure of progress, arguing that even intermittent treatment and reduced opioid use can lower the risk of opioid and injection-related harms. The low barrier approach adopted by the San Francisco Street Medicine Team is a step away from the traditional treatment models, which often aim for uninterrupted treatment and complete abstinence.
Key Takeaways and Future Directions: While the retention rates may appear modest, the outreach effort signifies a critical foothold in engaging homeless individuals with OUD—an accomplishment in its own right. The adaptability of the low barrier approach demonstrates that it is possible to make OUD treatment more accessible and tenable for the homeless population. Given the challenges in retention and overall treatment outcomes, future programs may benefit from additional resources such as housing, mental health services, and support for co-occurring substance use to improve their effectiveness.
Keywords
1. Buprenorphine treatment
2. Opioid Use Disorder
3. Homelessness
4. Heroin Addiction
5. Low barrier treatment
References
1. Carter Jamie J., Zevin Barry B., Lum Paula J. (2019). “Low barrier buprenorphine treatment for persons experiencing homelessness and injecting heroin in San Francisco.” Addiction Science & Clinical Practice. 14:20. doi:10.1186/s13722-019-0149-1.
2. Ahmad FB, et al. (2018). “Provisional drug overdose death counts.” National Center for Health Statistics. [Link]
3. Williams R, Nunes E, Olfson M. (2017). “To battle the opioid overdose epidemic, deploy the ‘cascade of care’ model.” Health Affairs Blog. [Link]
4. Mattick RP, et al. (2014). “Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence.” Cochrane Database Syst Rev. 2014;6(2):CD002207. doi: 10.1002/14651858.CD002207.pub4.
5. Sordo L, et al. (2017). “Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies.” BMJ. 2017;357:j1550. doi: 10.1136/bmj.j1550.
The study into low barrier buprenorphine treatment for San Francisco’s homeless heroin injectors signals an important advance in the field. Despite the challenges, the modest success underscores the necessity of flexible and inclusive strategies to address the deep-seated issues within this crisis. The hope is that with continued research and tailored interventions, society can move closer to a system that not only saves lives but also enhances them with sustained recovery and reintegration.