Liver cancer is a type of cancer that starts in the cells of your liver. The liver, which is a large organ located in the upper right part of your abdomen, has several functions, including detoxifying harmful substances in your body, storing vitamins and nutrients, producing bile to assist in digestion, and making proteins that help with blood clotting.
There are several types of liver cancer, but the most common type is called hepatocellular carcinoma (HCC). Other types include intrahepatic cholangiocarcinoma and hepatoblastoma, which mainly affects children.
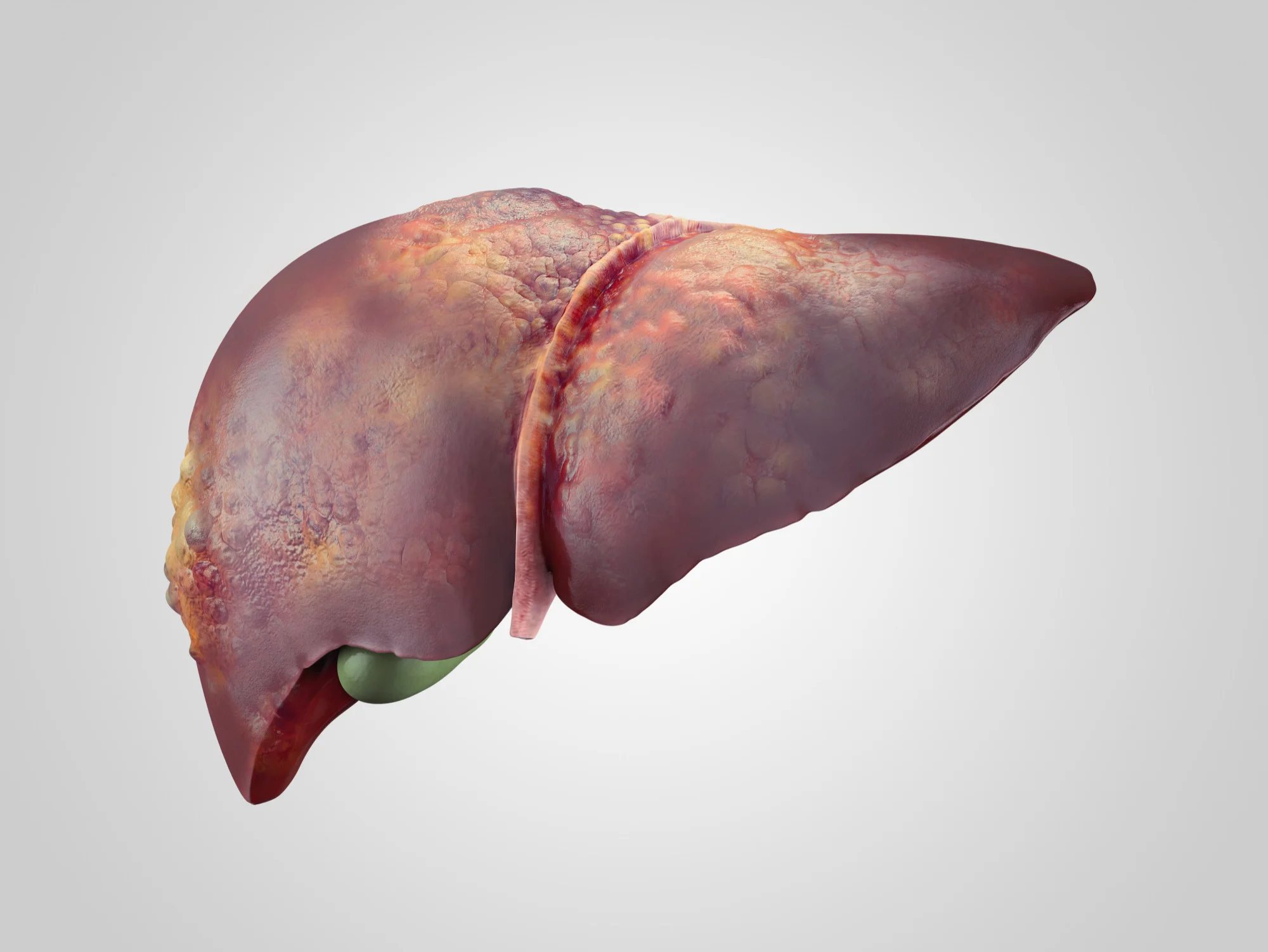
The exact cause of liver cancer is not known, however, several factors are known to increase the risk of developing the disease. Conditions like chronic hepatitis B or C infections, certain inherited liver diseases, diabetes, obesity, excessive alcohol consumption, exposure to certain chemicals, and long-term cirrhosis (scarring of the liver) are common risk factors.

The symptoms of liver cancer can be quite varied and in many cases, they don’t appear until the disease is quite advanced. Common symptoms include abdominal pain, jaundice (yellowing of the skin and eyes), unexplained weight loss, loss of appetite, nausea or vomiting, and fatigue.
Diagnosis of liver cancer typically involves a combination of blood tests, imaging studies like ultrasound, CT scans or MRI, and sometimes a liver biopsy.
Treatment options for liver cancer can vary, depending on the stage of the cancer, the overall health of the liver, and the patient’s overall health. Treatment options include surgery to remove the tumor, liver transplant, ablation therapy, radiation therapy, targeted therapy drugs, and immunotherapy.
Early detection and treatment of liver cancer can dramatically improve the patient’s prognosis, highlighting the importance of regular check-ups, especially for those with risk factors.
Causes of Liver cancer
Liver cancer happens when normal cells in the liver transform into abnormal cells and grow out of control. The specific cause of this transformation isn’t entirely understood, but there are certain factors that are known to increase the risk of developing liver cancer, including:
1. Chronic Hepatitis: The most common cause worldwide is chronic infection with hepatitis B or C virus. These infections lead to cirrhosis of the liver and changes in the cells, which can eventually result in liver cancer.
2. Cirrhosis: This irreversible and progressive condition causes scar tissue to form in your liver and increases your chances of developing liver cancer.
3. Certain inherited liver diseases: Diseases such as hemochromatosis and Wilson’s disease, where iron and copper accumulate in the liver, respectively, can increase the risk of liver cancer.
4. Diabetes: People with diabetes have a higher risk of liver cancer, especially if they also have other risk factors such as alcohol abuse or chronic viral hepatitis.
5. Non-alcoholic fatty liver disease: This condition, in which fat builds up in the liver, is most often seen in people who are overweight or obese or have type 2 diabetes.
6. Aflatoxins: Aflatoxins, which are produced by fungi, are known to cause liver cancer. These toxins can contaminate crops like peanuts and corn, which are dietary staples in some parts of the world.
7. Alcohol abuse: Alcohol abuse is a common cause of cirrhosis, which can lead to liver cancer.
8. Smoking: Smoking can increase the risk of liver cancer, especially in those who abuse alcohol or have chronic viral hepatitis.
Remember, while these factors increase the risk of liver cancer, they do not necessarily cause liver cancer. Not everyone with these risk factors will develop this disease.
Risk Factors of Liver cancer
Liver cancer risk factors include:
1. Cirrhosis: This progressive and irreversible condition causes scar tissue to form in your liver and increases your chances of developing liver cancer.
2. Certain liver diseases: Hepatitis B virus (HBV) or Hepatitis C virus (HCV) infections can significantly increase the risk of liver cancer.
3. Diabetes: People with this blood sugar disorder have a greater risk of liver cancer than those who don’t have diabetes.
4. Non-alcoholic fatty liver disease: Fat buildup in the liver increases the risk of liver cancer.
5. Chronic alcohol consumption: Drinking alcohol every day over many years can lead to irreversible liver damage and increase the risk of liver cancer.
6. Specific inherited liver diseases: Diseases, such as hemochromatosis and Wilson’s disease, can increase liver cancer risk.
7. Exposure to aflatoxins: Aflatoxins are poisons produced by molds that grow on crops that are stored poorly. Consumption of these crops can increase the risk of liver cancer.
8. Certain rare diseases: Diseases like alpha-1 antitrypsin deficiency, tyrosinemia, and glycogen storage diseases can increase liver cancer risk.
9. Older age: The majority of people diagnosed with liver cancer are over the age of 63.
10. Obesity: Being obese can increase the risk of liver cancer.
It’s important to note that having one or more of these risk factors does not guarantee the development of liver cancer. Similarly, individuals may develop liver cancer even without having any of these risk factors. Regular check-ups and early detection play a key role in effectively managing and treating liver cancer. Always consult with healthcare professionals for personalized advice.
Signs and Symptoms of Liver cancer
Liver cancer does not usually have obvious symptoms in the early stages, but as it progresses it can cause the following:
1. Jaundice: This is a yellowing of the skin and eyes due to the build up of a substance called bilirubin in the blood. It can cause itchy skin, dark urine, and light-colored stools.
2. Abdominal Pain: This might be located in the upper-right portion of the abdomen.
3. Swollen abdomen or bloating: This could be caused by a buildup of fluid in the abdomen called ascites.
4. Loss of appetite or sudden weight loss: Individuals may experience a loss of appetite or feel full after small meals.
5. Nausea and vomiting: These might be more consistent and severe than typical feelings of nausea or digestion problems.
6. Fatigue or weakness: Patients might feel unusually tired or weak.
7. Chronic liver disease: Liver cancer usually happens due to chronic liver diseases like cirrhosis, hepatitis B or C. In this case, the related symptoms like bruising or bleeding easily, chronic fatigue, poor appetite, or having a buildup of fluid in your abdomen.
8. White, chalky stools: If the cancer is blocking the bile duct, you might have bowel movements that are white or chalky.
If you notice any of these signs or symptoms, you should consult with a healthcare professional immediately as they could be the sign of liver cancer or another serious condition. Please note these symptoms can also relate to other conditions, so do not panic but do seek medical advice.
Diagnosis Liver cancer
Liver cancer is a type of malignancy that begins in the cells of your liver. The liver is a large organ at the top right side of your abdomen. It has vital functions including detoxifying harmful substances in your body, storing vitamins and nutrients, producing bile to aid digestion, and producing proteins that help your blood clot.
Several types of cancer can form in the liver. The most common type of liver cancer is hepatocellular carcinoma, which begins in the main type of liver cell called hepatocyte. Other types of liver cancer, like intrahepatic cholangiocarcinoma and hepatoblastoma, are much less common.
Not all cancers that affect the liver are considered liver cancer. Cancers that begin in other parts of the body, such as the colon, lung, or breast, can also spread (metastasize) to the liver. These types of cancers are named after the organ in which they began. For instance, colon cancer that spreads to the liver is referred to as metastatic colon cancer, and not liver cancer.
The diagnosis of liver cancer usually consists of a physical examination, review of patient’s history, lab tests including blood tests, imaging tests such as CT scan, MRI, or ultrasound of the liver, and sometimes a liver biopsy where a sample of tissue is taken from the liver and examined under a microscope.
Symptoms of liver cancer often do not show up until the later stages of the disease, but may include weight loss, loss of appetite, upper abdominal pain, nausea and vomiting, general weakness and fatigue, swelling in the abdomen, and yellow discoloration of your skin and the whites of your eyes (jaundice).
The exact cause of liver cancer is still unknown, but several factors have been linked to the disease, including chronic infection with certain viruses (such as hepatitis B and C), cirrhosis, certain inherited liver diseases, diabetes, obesity, and excessive alcohol consumption.
Treatment of Liver cancer
Liver cancer is a complex condition that requires a multi-modal approach to treatment. The course of treatment depends on several factors including the patient’s overall health, the size and location of the tumor(s), and whether the cancer has spread to other parts of the body. Here are some common treatment options:
1. Surgery: This is often the first line of treatment if the cancer is localized and the patient is in good overall health. The surgeon may remove a portion of the liver where the cancer is located (a procedure known as a partial hepatectomy), or if the disease is advanced, a liver transplant may be considered.
2. Ablation Therapy: Ablation techniques destroy tumor cells by applying extreme heat (radiofrequency ablation) or cold (cryoablation) to the cancerous tumors. This approach is often used for smaller tumors or for patients who cannot undergo surgery.
3. Embolization Therapy: This involves injecting substances to cut off the blood supply to the cancer cells. When the cells are deprived of oxygen and nutrients, they die. This treatment includes chemoembolization (delivering chemotherapy drugs directly to the liver), radioembolization (delivering radiation directly to the liver), and bland embolization (which uses microscopic spheres to block the blood supply to the tumors).
4. Targeted Therapy: These drugs work by specifically attacking certain parts of cancer cells. They can help slow the growth of tumors or shrink them.
5. Immunotherapy: This treatment approach boosts the body’s natural defenses to fight the cancer. It may involve using substances made by the body or in a lab that enhances or restores immune system function.
6. Radiation Therapy: External radiation can be used to kill cancer cells in the liver. This is often done in combination with other treatments.
7. Chemotherapy: Traditional chemotherapy uses drugs to kill cancer cells or stop them from dividing. But given the liver’s role in detoxifying the body, systemic chemotherapy (chemotherapy delivered via the bloodstream to the entire body) is often less effective in treating liver cancer.
Every case of liver cancer is unique, so treatment plans will need to be tailored to each patient’s situation. Always it’s important for patients to discuss all treatment options, along with their benefits and risks, with their healthcare providers in order to make the best decisions for their care.
Medications commonly used for Liver cancer
Liver cancer is often treated with a multi-modal approach, which includes surgery, radiation, and medication. Certain types of medicines used for liver cancer include:
1. Chemotherapy Drugs: These are drugs that kill cancer cells or prevent them from growing. Common chemotherapy drugs used for liver cancer include Sorafenib (Nexavar), Lenvatinib (Lenvima), and Regorafenib (Stivarga).
2. Immunotherapy Drugs: These medicines harness the power of the immune system to fight cancer. Nivolumab (Opdivo) and Pembrolizumab (Keytruda) are immunotherapy drugs that are sometimes used in cases of advanced liver cancer.
3. Targeted Therapy Drugs: These drugs specifically target the changes in cells that cause them to become cancerous. For liver cancer, a targeted therapy might be used to block the growth of new blood vessels that tumors need to grow. Examples include Bevacizumab (Avastin) and Ramucirumab (Cyramza).
4. Radiation-sensitizing Drugs: These drugs make cancer cells more susceptible to the effects of radiation therapy.
5. Hepatoprotective Drugs: These drugs are used to protect the liver from damage that can be caused by chemotherapy and other medications.
The type of medication used in each case will depend on the specific characteristics of the cancer and the overall health of the patient. It’s also possible that a combination of these medications might be used.
Please note, while this list contains the most commonly used medications, it’s not comprehensive and there are other drugs that may be recommended in certain situations. Always consult your physician or healthcare professional for personalized treatment advice.
Prevention of Liver cancer
Preventing liver cancer involves a combination of lifestyle modifications and regular medical check-ups. Here are some effective steps to potentially reduce the risk of developing liver cancer:
1. Limit Alcohol Intake: Chronic, heavy alcohol consumption can lead to cirrhosis, which in turn can lead to liver cancer. So reduce your alcohol intake.
2. Avoid Exposure to Certain Toxins: Substances such as aflatoxins produced by molds on crops can cause liver cancer. Limit your consumption of such affected crops and ensure your food is stored appropriately to avoid the growth of such molds.
3. Maintain a Healthy Weight: Being overweight or obese increases the risk of non-alcoholic fatty liver disease and cirrhosis, both of which might lead to liver cancer. Therefore, maintain a healthy body weight and exercise regularly.
4. Get Vaccinated: Getting vaccinated against diseases like Hepatitis B and Hepatitis C reduces the risk of liver diseases and thus, liver cancer.
5. Avoid Risky Behaviors: Engaging in risky behaviors like intravenous drug use or unprotected sex can indirectly lead to liver cancer by increasing the risk of hepatitis infection.
6. Regular Check-Ups: Regular medical check-ups can help in the early detection and treatment of liver diseases, reducing the risk of liver cancer. Individuals with chronic liver diseases should be monitored more closely for early signs of liver cancer.
7. Healthy Diet: Consuming a diet high in fruits and vegetables and low in fats, sugars and processed foods can help avoid obesity and non-alcoholic fatty liver disease, which may lower the risk of liver cancer.

Remember that these measures can only reduce the risk, they can’t eliminate the possibility of developing liver cancer entirely. As always, seek advice from healthcare professionals for personalized recommendations.
FAQ’s about Liver cancer
1. What is liver cancer?
Liver cancer is the abnormal growth of cells in the liver.
2. What are the types of liver cancer?
There are two main types of liver cancer: Hepatocellular carcinoma (HCC) and cholangiocarcinoma. HCC is more common, and it originates in the liver cells themselves. Cholangiocarcinoma, less common, starts in the bile ducts.
3. What are the risk factors for liver cancer?
Factors that increase the risk of liver cancer include chronic infection with hepatitis B or C, cirrhosis, certain inherited liver diseases, diabetes, obesity, and exposure to aflatoxins (a toxin produced by fungus that can contaminate crops).
4. What are the symptoms of liver cancer?
Symptoms can include fatigue, feeling full quickly, loss of appetite, abdominal pain or swelling, yellowing of the skin and eyes (jaundice), nausea and vomiting, and white, chalky stools.
5. How is liver cancer diagnosed?
Liver cancer is typically diagnosed through medical history, physical examination, blood tests, imaging tests (like a CT scan or MRI), and a liver biopsy.
6. What are the treatment options for liver cancer?
The course of treatment varies based on the size, location, and stage of the cancer as well as the patient’s overall health. Options can include surgery, liver transplant, ablative therapies, radiation therapy, targeted therapy, immunotherapy, and chemotherapy.
7. What is prognosis for liver cancer?
Prognosis for liver cancer varies greatly depending on the stage of the cancer at the time of diagnosis and the overall health of the patient. Early-stage liver cancer that is removed completely during surgery has the best prognosis.
8. Can liver cancer be prevented?
While it’s not completely preventable, risk can be lowered by preventing hepatitis B and C infections, maintaining a healthy weight, controlling diabetes, and avoiding heavy alcohol use.
9. How common is liver cancer?
According to the American Cancer Society, liver cancer is the fifth most common cause of cancer death in men and the ninth in women.
Disclaimer: This information is for general understanding. If you or anyone has any medical concerns or symptoms, they should consult with a healthcare professional.
Useful links
Liver cancer is a serious condition where abnormal cells grow uncontrolled in the organ’s tissues. There are two primary types – hepatocellular carcinoma (HCC), the most common, and cholangiocarcinoma. Causes may include chronic liver diseases like hepatitis or cirrhosis, alcohol abuse, and certain inherited liver diseases. Symptoms may include abdominal pain, unexplained weight loss, yellowish skin, and swelling in the abdomen.
Below are some resources for further information about liver cancer from reputable scientific journals and healthcare organizations:
Please consult your doctor or a healthcare professional for more personalized information on this topic and specific advice about treatment options.
Complications of Liver cancer
Liver cancer can present a number of complications, both from the disease itself and from the treatments used to manage it. Here are some of them:
1. Cirrhosis: Many people with liver cancer also have cirrhosis, a scarring of the liver tissue. This can make treatment more difficult and the prognosis worse. Cirrhosis can lead to other complications like fluid accumulation in the abdomen (ascites) and confusion or coma (hepatic encephalopathy).
2. Liver Failure: Liver cancer may progress to the point where the liver can no longer perform essential functions, leading to liver failure. Symptoms might include jaundice (yellowing of the skin and eyes), ascites, and eventually coma.
3. Spread of Cancer (Metastasis): Liver cancer can spread (metastasize) to other parts of the body, such as the lungs, bones, and lymph nodes, creating additional health problems.
4. Portal Hypertension: This is increased blood pressure in the veins that bring blood to the liver. It can lead to varices (swollen blood vessels) in the esophagus or stomach, which can bleed heavily.
5. Bleeding or Hemorrhage: Tumors can grow into the blood vessels of the liver and cause bleeding, either into the liver (hematoma) or into the abdominal cavity (hemoperitoneum).
6. Side Effects from Treatment:
Surgery: Potential complications include infections, bleeding, and harm to nearby organs.
Chemotherapy: Can cause nausea, vomiting, hair loss, fatigue, infections, and more. Some chemotherapy drugs can also harm the healthy parts of the liver.
Radiation Therapy: Can damage healthy nearby organs and tissues, and may cause nausea, vomiting, fatigue, skin changes, and other side effects.
Targeted Therapy and Immunotherapy: These therapies might also lead to various side effects including rash, diarrhea, liver inflammation (hepatitis), flu-like symptoms, fatigue, and others.
7. Pain: The cancer itself and some treatments can cause discomfort or pain.
Please note that not all patients will experience these complications and different patients respond to treatments in different ways. The potential risks and advantages should be discussed with the healthcare team.
Home remedies of Liver cancer
While it is crucial to note that no home remedy can cure liver cancer and that a proper medical treatment plan is essential, certain lifestyle changes and home remedies can support liver health and complement cancer treatment:
1. Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats contributes to overall health, boosting your immune system and helping you better resist illness.
2. Regular Exercise: Regular physical activity helps maintain a healthy weight, boost mood and energy, and contribute to overall health.
3. Water: Staying hydrated is essential to flush toxins from the body.
4. Limit Alcohol: Alcohol can be harmful to your liver.
5. Milk Thistle: This herb is believed to have liver-protecting effects, though scientific evidence is limited. Consult with a healthcare provider before starting any herbal supplement.
6. Green Tea: It contains antioxidants that could protect the liver, though more research is needed.
7. Avoid Toxins: Avoid chemicals, such as those in cleaning products, insecticides, and more. They can damage the liver.
8. Practice Safe Sex: Hepatitis B and C can be transmitted sexually. These viral infections are major risk factors for liver cancer.
9. Regular Check-ups: Regular check-ups and screenings can catch liver cancer early when treatment is more likely to be successful.
10. Meditation and Stress Reduction: Techniques like yoga, massage, mindfulness can help manage stress.
However, it is important to note that none of these home remedies can cure liver cancer. They serve to improve your overall well-being.
PLEASE consult with your healthcare provider or a registered dietitian before starting any home remedies, diets, or exercises, especially if you are diagnosed with liver cancer. Cancelling or delaying the standard cancer treatments can have life-threatening consequences. Discuss any complementary therapies or lifestyle changes you are interested in with your doctor to ensure they are safe and won’t interfere with your treatment.