Hepatitis C is a viral infection that causes liver inflammation, sometimes leading to serious liver damage. The hepatitis C virus (HCV) is spread through contaminated blood, which may happen through needle sharing, unsterilized medical equipment, or unscreened blood transfusions.
It can range in severity, being a ‘mild illness’ that lasts a few weeks, to a ‘serious, lifelong illness’. Some people, when first infected, may have mild symptoms like fatigue, while others may have no symptoms at all.
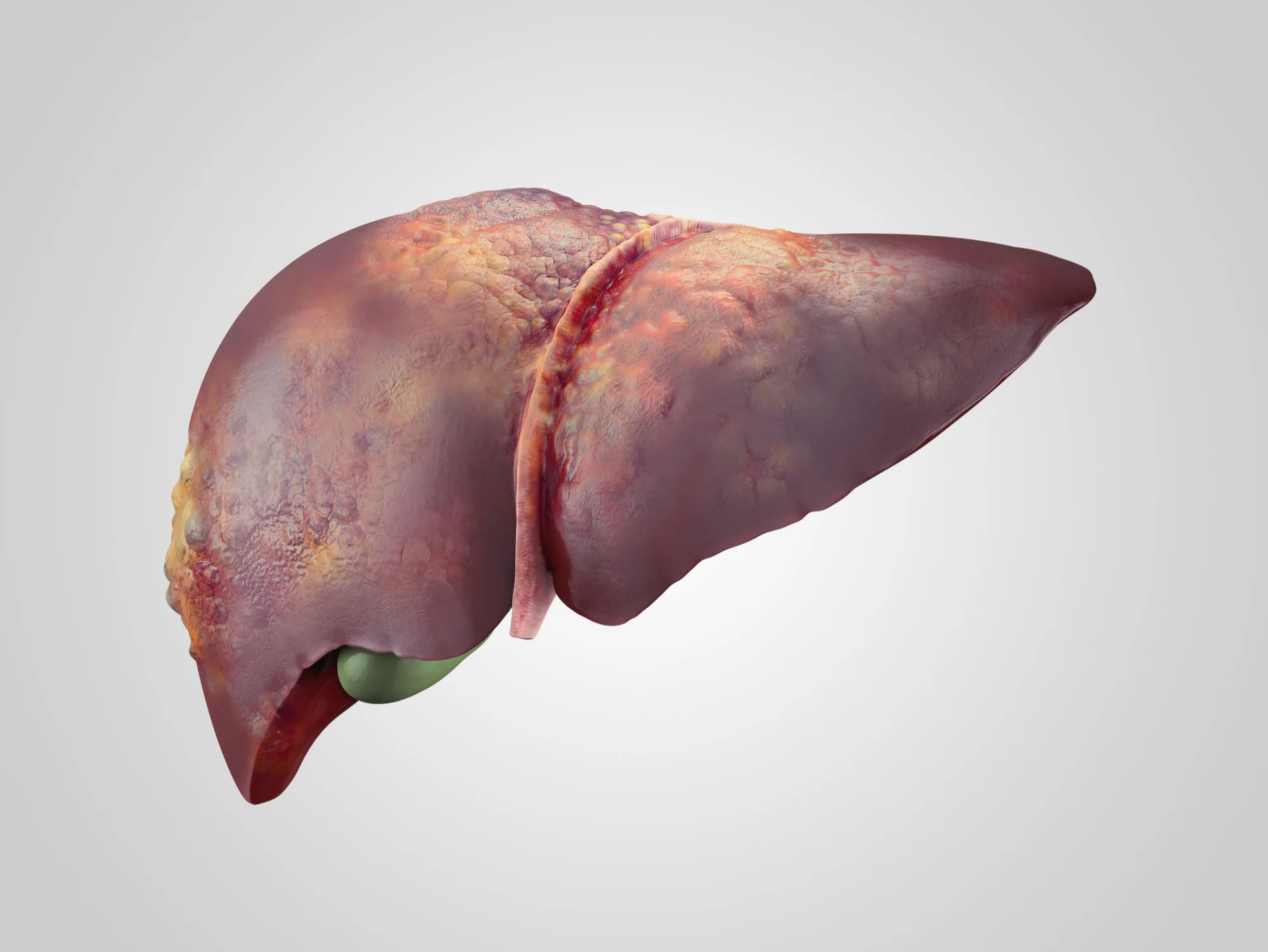
Chronic Hepatitis C infection can lead to severe complications like cirrhosis, liver failure, or liver cancer over a period of decades. There are treatments available that can cure Hepatitis C infection and prevent these complications. These treatments typically involve antiviral medications.

Hepatitis C is often asymptomatic, which means it often goes undetected until liver damage shows up on routine medical tests. For this reason, it’s often called the “silent epidemic.” It is a major cause of liver cirrhosis and liver cancer.
Prevention measures include safe handling of needles and syringes, testing donated blood for hepatitis C, and practicing safer sex behaviors.
Causes of Hepatitis C
Hepatitis C is primarily caused by the Hepatitis C virus (HCV), which is spread or transmitted through direct contact with contaminated blood. Some of the primary means through which this transmission takes place are:
1. Blood transfusions and organ transplants: Before widespread screening of blood began in 1992, this was a common way Hepatitis C was spread.
2. Shared needles: Sharing IV drug paraphernalia, including needles, is presently the most common mode of transmission of Hepatitis C in the United States.
3. Needlestick injuries: Healthcare workers are at risk through exposure to infected blood, particularly via accidental needlestick injuries.
4. Birth: Mothers who have Hepatitis C can pass on the virus to their babies during childbirth.
5. Tattooing and piercing: If tools aren’t properly sterilized, they can cause transmission if used on multiple people.
Less commonly, the virus can be transmitted through sexual contact or sharing personal items such as razors or toothbrushes that might have come into contact with an infected person’s blood.
It’s important to note that Hepatitis C can’t be spread through casual contact, like shaking hands, sharing eating utensils, or through food and water.
Risk Factors of Hepatitis C
Hepatitis C is a viral infection that causes liver inflammation, sometimes leading to severe liver damage. The hepatitis C virus (HCV) spreads through contaminated blood. Here are some risk factors associated with the contracting of hepatitis C:
1. Blood transfusions or organ transplants: Before 1992, when widespread screening of the blood supply began in the United States, blood transfusions and organ transplants were a major source of hepatitis C infection.
2. Shared needles: Sharing intravenous drug paraphernalia puts you at high risk of hepatitis C.
3. Needlestick injuries: Healthcare workers are at risk for hepatitis C due to needlestick injuries.
4. Unprotected sexual intercourse: Unprotected sex with someone infected with HCV increases the risk, especially if you have multiple sexual partners, a sexually transmitted infection, or HIV.
5. Tattooing or piercing: Unregulated tattooing or piercing where equipment hasn’t been properly sterilized can pose a risk
6. HIV infection: If you’re HIV-positive, you’re more susceptible to hepatitis C.
7. Birth: Mothers infected with the hepatitis C virus can pass the virus to their offspring during childbirth.
8. Dialysis: People who undergo long-term kidney dialysis can contract hepatitis C.
Most people with acute hepatitis C do not experience symptoms, so getting tested is crucial if you’re at risk. If left untreated, chronic hepatitis C can lead to cirrhosis, liver cancer, liver failure, or other health problems.
Signs and Symptoms of Hepatitis C
Hepatitis C is a viral infection that primarily affects the liver. Often, it may present no symptoms, especially in the early stages. When symptoms do occur, they may take several weeks or even months to appear after exposure. Below are some signs and symptoms:
1. Fever: This is among the early symptoms of Hepatitis C, though it is not very common.
2. Fatigue: A person with Hepatitis C often feels unusually tired, even without physical exertion.
3. Decrease in appetite: There can be a significant loss in appetite that could lead to weight loss.
4. Nausea and vomiting: This is more common in more advanced stages of the disease.
5. Abdominal pain: Discomfort or pain in the stomach area is another common symptom. This happens as the liver is inflamed.
6. Dark urine: Hepatitis C can cause the color of your urine to darken due to the excess bilirubin in the bloodstream, which the liver cannot properly filter.
7. Jaundice: This symptom appears as a yellow coloration of the skin and the whites of the eyes. This is caused by a buildup of bilirubin, a yellowish pigment, in the bloodstream.
8. Itchy skin: Some people with hepatitis C might have symptoms of pruritus, or intense itchy skin.
9. Swelling in the legs: This symptom, also known as edema, may appear during advanced stages due to liver damage.
10. Confusion, drowsiness and slurred speech: These symptoms can occur in later and more serious stages of hepatitis C, due to the buildup of toxins in the bloodstream that the damaged liver can no longer effectively remove.
These symptoms are not exclusively linked to Hepatitis C and can be associated with other conditions. The best way to confirm a Hepatitis C infection is through a blood test. If you think you might have been exposed to the virus or have any of the symptoms, it’s important to see your doctor.
Diagnosis Hepatitis C
Hepatitis C is a viral infection that primarily affects the liver, leading to its inflammation and damage. It is caused by the Hepatitis C virus, which is usually transmitted through direct contact with the blood of a person who has the disease. This can occur through sharing drug injection equipment, receiving contaminated blood transfusions or organ transplants, or sometimes from mother to baby during birth.
There are two types of hepatitis C: acute and chronic. Acute Hepatitis C is a short-term illness that occurs within the first 6 months after someone is exposed to the virus. Most acute cases become chronic infections.
Chronic Hepatitis C is a long-term illness that happens when the virus remains in a person’s body. Chronic hepatitis C can eventually cause serious health problems like liver cancer or cirrhosis.
Diagnosis of Hepatitis C is usually done via blood tests to look for antibodies to the virus or to identify genetic material (RNA) of the virus itself. If there is suspicion of liver damage, further tests such as a liver function test or liver biopsy may be done.
It’s very important to know your diagnosis as early as possible because many people can have Hepatitis C without symptoms until major liver damage has occurred. Nowadays, treatment options are very effective and can cure most people with the disease.
Treatment of Hepatitis C
Hepatitis C is a viral infection that causes liver inflammation and damage. Long-term hepatitis C can lead to severe health problems, including liver cancer and cirrhosis.
Treatment for Hepatitis C includes the following:
1. Antiviral Medications: These are prescribed to prevent the virus from multiplying in the body, which helps to slow the progression of liver disease. The choice of medication and duration of treatment depend on the type of hepatitis C virus, the extent of liver damage, other health conditions, and whether a patient has been treated for hepatitis C before. Current treatments usually involve 8–24 weeks of oral therapy and can cure more than 90% of people with hepatitis C.
2. Liver Transplant Surgery: In severe cases where the liver has been significantly damaged, a liver transplant might be the best option. This is usually considered when hepatitis C has progressed to cirrhosis or liver cancer. However, the new liver can still become infected with the virus.
3. Vaccination: There’s no vaccine for Hepatitis C, but doctors usually recommend patients with the virus to receive vaccines for Hepatitis A and B to prevent coinfection and further liver damage.
4. Healthy Lifestyle Choices: Patients are advised to avoid alcohol and substances that can cause further liver damage. Regular exercise, a balanced diet, and maintaining a healthy weight can also help manage Hepatitis C.
While these treatments can cure most people with Hepatitis C, the virus can return if the patient is exposed again. Regular follow-ups with healthcare providers and routine tests will help monitor the disease’s progress and treatment effectiveness.
Always consult your healthcare provider for your individual treatment options. It’s important to note that many people with chronic hepatitis C don’t know they have it because they have no symptoms, so regular screening becomes essential for high-risk people.
Medications commonly used for Hepatitis C
Hepatitis C is typically treated with antiviral medications intended to clear the virus from your body. The aim of treatment is to have no hepatitis C virus detected in your body at least 12 weeks after you complete treatment. Here are some commonly used medications for Hepatitis C:
1. Harvoni (Ledipasvir/Sofosbuvir): It is a combination of two antiviral medications used to treat chronic (long-lasting) hepatitis C.
2. Sovaldi (Sofosbuvir): It prevents the virus that causes hepatitis C from multiplying in your body. Sovaldi is a key component in several combination treatments, providing a backbone for the regimen.
3. Zepatier (Elbasvir and Grazoprevir): Another combination of two distinct antiviral drugs, Zepatier is employed for chronic hepatitis C, genotypes 1 and 4.
4. Viekira Pak (Ombitasvir/Paritaprevir/Ritonavir (dasabuvir)): This is a multi-drug regimen used for specific types of Hepatitis C.
5. Ribavirin: It is an antiviral medication that prevents hepatitis C virus (HCV) cells from multiplying in your body.
6. Epclusa (Sofosbuvir/Velpatasvir): A combination of two antiviral medications, it is used to treat chronic hepatitis C in adults.
7. Mavyret (Glecaprevir/Pibrentasvir): It is an antiviral medication used to treat all six genotypes of hepatitis C in adults without cirrhosis or with compensated cirrhosis.
Each medication has its own list of potential side effects, benefits, and contraindications. These medications are often taken for several weeks to months, and one or more may be recommended based on the type of hepatitis C, the individual’s other health conditions, and the individual’s response to therapy. As with all medications, these should only be taken under the guidance of a healthcare provider.
Prevention of Hepatitis C
Hepatitis C is a viral infection that causes liver inflammation and can potentially lead to serious liver damage. There is no vaccine for hepatitis C, but several measures can help prevent its spread:
1. Avoid Sharing Needles: Sharing drug needles is the most common way that hepatitis C spreads. Never share needles, syringes, or other drug-related equipment.
2. Practice Safe Sex: Although the risk of getting hepatitis C from sexual intercourse is low, the risk increases if you have multiple sex partners, have a sexually transmitted disease, or are engaging in rough or unprotected sex. Therefore, always practice safe sex.
3. Be Careful When Getting Tattoos or Piercings: Make sure that the tattoo or piercing shop uses sterile needles and inks. Poor infection control in these settings can lead to the disease spreading.
4. Avoid Sharing Personal Items: Never share personal items that can have blood on them, like razors, toothbrushes, or nail clippers.
5. Practice Healthcare Precautions: If you’re a healthcare worker, always follow proper protocol for handling needles and other sharp objects.
6. Screening for Blood Transfusions and Organ Transplants: In many countries including the United States, screening for hepatitis C is done for all donated blood, blood products, and organs to prevent hepatitis C transmission.
Finally, if you think you are at risk for Hepatitis C or if you may have been exposed, you should get tested. Early diagnosis can prevent the disease from progressing and causing further damage.
FAQ’s about Hepatitis C
Hepatitis C is a viral infection that primarily affects the liver. Here are some frequently asked questions (FAQs) about Hepatitis C.
1. What is Hepatitis C?
Hepatitis C is a liver disease caused by the Hepatitis C virus (HCV). It can lead to both acute and chronic infections.
2. How is Hepatitis C transmitted?
Hepatitis C is primarily transmitted through exposure to small quantities of blood. This can happen through injection drug use, unsafe injection practices, unsafe health care, blood transfusion, and sexual practices that lead to blood exposure.
3. What are the symptoms of Hepatitis C?
Many people with Hepatitis C do not experience symptoms and are unaware of their infection. However, some people may experience symptoms such as fatigue, loss of appetite, nausea, vomiting, abdominal pain, and jaundice.
4. How is Hepatitis C diagnosed?
Hepatitis C is diagnosed through blood tests, which can detect anti-HCV antibodies or the HCV genome.
5. Is there a cure for Hepatitis C?
Yes, Hepatitis C can be cured with antiviral medications, which eliminate the virus from the body and prevent liver damage.
6. Can Hepatitis C be prevented?
There is currently no vaccine for Hepatitis C, however, it can be prevented by avoiding behaviors that can spread the disease, particularly injecting drugs.
7. What is the treatment for Hepatitis C?
The goal of the Hepatitis C treatment is to cure the person from the virus. The most commonly used medications for treating Hepatitis C are known as direct-acting antivirals.
8. Can you get Hepatitis C more than once?
Yes, having been infected with Hepatitis C once does not protect you from getting the virus again.
9. How common is Hepatitis C?
According to the World Health Organization, in 2015, an estimated 71 million people were living with chronic Hepatitis C infection worldwide.
10. Is it possible to have Hepatitis C without knowing it?
Yes. Because many people with Hepatitis C don’t have symptoms, they may not know they have it until a routine blood test shows liver damage.
Useful links
Hepatitis C is a viral infection that causes liver inflammation, often leading to severe liver damage. The hepatitis C virus (HCV) spreads through contaminated blood. Chronic Hepatitis C is usually a “silent infection” for many years, until the virus damages the liver enough to cause the signs and symptoms of liver disease.
Here are some useful links from journals and medical resources with regards to Hepatitis C:
Remember to consult with healthcare providers when seeking medical advice or treatment. These articles are intended to provide general understanding and knowledge about Hepatitis C, but do not replace professional medical advice.
You could also access the Centers for Disease Control (CDC) for additional information related to Hepatitis C: https://www.cdc.gov/hepatitis/hcv/index.htm
Complications of Hepatitis C
Hepatitis C, a viral infection that primarily affects the liver, can cause several complications if it’s not properly managed or treated. They include:
1. Chronic liver disease: Approximately 75%-85% of people who get infected with Hepatitis C will develop a chronic liver disease.
2. Cirrhosis: About 20%-30% of people suffering from chronic Hepatitis C will develop cirrhosis, i.e., scarring of the liver. This could take about 20 to 30 years to develop from the onset of the infection.
3. Liver cancer: People with chronic Hepatitis C and cirrhosis have a higher risk of developing liver cancer.
4. Liver failure: Advanced cirrhosis can cause your liver to stop functioning, also known as liver failure. This is a life-threatening condition and typically requires a liver transplant.
5. Extrahepatic complications: Hepatitis C is also associated with diseases outside the liver, including skin rashes, arthritis, diabetes, certain infections, kidney disease, depression, and lymphoma.
6. Hepatic encephalopathy: This is a decline in brain function that happens as a result of severe liver disease.
It’s important to remember that these complications can be avoided or significantly delayed by early diagnosis and treatment of Hepatitis C. Current treatments are very effective and can cure the disease in most cases.
Home remedies of Hepatitis C
While there’s no specific home remedy or cure for Hepatitis C, certain lifestyle changes and natural remedies can help manage symptoms and protect your liver. However, these should never replace the medical treatment plan recommended by your healthcare provider. They can include:
1. Healthy Diet: Consuming a balanced diet that’s high in fruits, vegetables, and lean proteins can improve your overall health.

2. Drink Plenty of Fluids: Water helps the liver process toxins and can help relieve some symptoms such as fatigue.
3. Regular Exercise: Regular physical activity can boost the immune system and help maintain a healthy weight, which is essential in overall liver health.
4. Avoid Alcohol: Alcohol can cause further liver damage, making your symptoms worse. Hence, it’s critical to abstain from alcohol entirely.
5. Avoid Certain Medications: Some over-the-counter medicines and herbs can cause liver damage – always consult with your doctor.
6. Reduce Stress: Techniques such as meditation, yoga, and deep breathing can help manage stress and improve wellbeing.
7. Green Tea: Some studies suggest that green tea can have beneficial effects on the liver.
8. Coffee: Studies demonstrate that drinking coffee can help to slow down the progression of liver disease in some people.
Remember, Hepatitis C is a serious medical condition that requires appropriate medical treatment. Simply managing symptoms using at-home methods isn’t enough – it’s crucial to follow the treatment regimen your doctor prescribes to combat the virus and limit liver damage. This most often includes antiviral medications.
This information is provided as a guide and for informational purposes only and is not intended as medical advice. For accurate information, always consult with a healthcare provider.