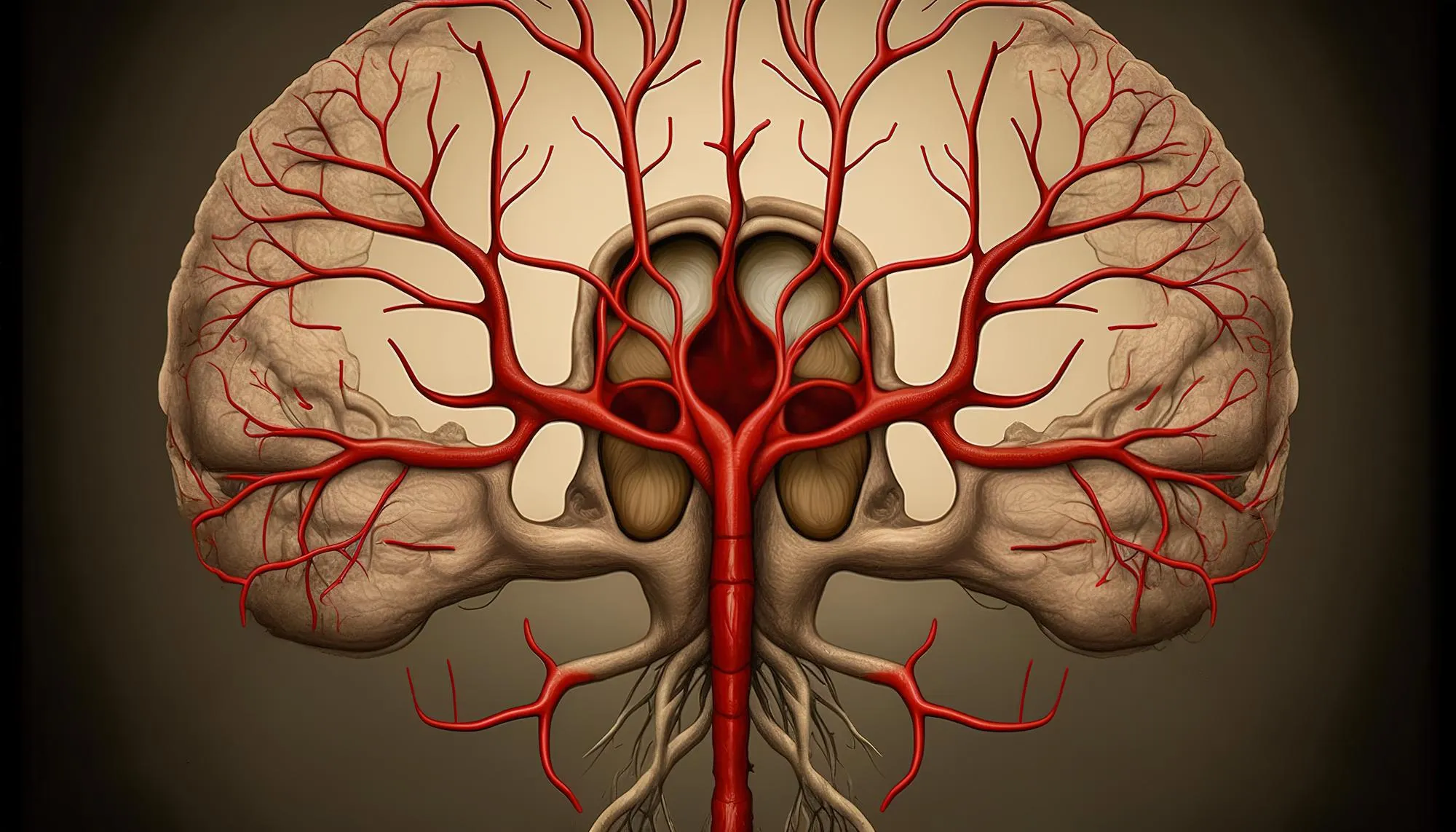
The medical field continues to face complex cases that test the boundaries of our understanding. One such example is the rare and perplexing condition known as primary angiitis of the central nervous system (PACNS), which poses significant challenges during diagnosis and treatment. This case report, derived from an article published by Wada Takafumi et al., in the Japanese journal Rinsho Shinkeigaku, sheds light on a complex presentation of PACNS involving cerebral infarction and spinal hemorrhage, and underscores the importance of distinguishing it from reversible cerebral vasoconstriction syndrome (RCVS).
Patient Presentation
A 61-year-old woman was admitted to the Department of Neurology at Kurashiki Central Hospital with acute intense lower back pain and a debilitating weakness in her left leg. Concurrently, she suffered from a throbbing headache. Upon examination, she exhibited several neurological deficits, including muscle weakness in the left leg, lower left quadrantanopia—a partial loss of vision—and left lower extremity deep sensory disturbance.
Laboratory Findings and Imaging
The initial laboratory data provided no evidence of coagulopathy, and autoimmune antibody levels were within normal ranges. However, a cerebrospinal fluid examination presented both bloody and inflammatory indicators. Advanced imaging techniques, including brain and spinal magnetic resonance imaging (MRI), revealed a cerebral infarction characterized by multiple intracranial arterial stenosis and a convexal subarachnoid hemorrhage. Further scans identified spinal hemorrhage affecting the cervical, thoracic, and parts of the lumbar spine.
Based on the synchronous occurrence of these lesions, the medical team led by Takafumi Wada, along with colleagues Hiroshi Kitaguchi and Katsuro Shindo at the same department made a challenging diagnosis of vasculitis, specifically PACNS.
Differential Diagnosis and Treatment
The initial presentation of PACNS can be easily confused with that of RCVS, especially since the two disorders share similar initial symptoms and examination findings. Notably, though, treatment and prognosis differ markedly between the two. After the administration of high-dose corticosteroids therapy, the patient under discussion showed improvement in the multiple arterial stenosis.
The successful outcome for this patient underscores the critical role of differential diagnosis in neurological conditions that present with angiitis. The treatment regimen typically includes administration of immunosuppressive agents, such as methylprednisolone and prednisolone, which were used in this case. The dosage and duration of therapy are determined based on the severity of the condition and response to the initial treatment.
Implications for Clinical Practice
This case report serves as a crucial reminder of the complexities involved in the diagnosis and management of PACNS. It highlights the need for a thorough and methodical approach when dealing with symptoms suggestive of cerebral vasculitis and the value of advanced imaging diagnostics in detecting and confirming the presence of this rare disorder.
While this patient’s case concluded with a favorable outcome, due to the elusive nature of PACNS, clinicians must remain vigilant for this potential diagnosis, particularly in patients presenting with a combination of neurological deficits, cerebrospinal fluid abnormalities, and MRI findings indicative of angiitis.
Conclusion
Primary angiitis of the central nervous system is a rare, yet challenging, diagnosis that demands a high degree of clinical suspicion and astuteness. The case discussed herein provides a critical example of how multifaceted and nuanced the presentation of PACNS can be, how it can mimic other conditions like RCVS, and how prompt and appropriate treatment can lead to substantial improvements in patient outcomes.
Physicians should take note of this case as a guide for managing similar presentations of neurological disorders, keeping in mind that individual patients may exhibit unique clinical features that require personalized treatment strategies. Moreover, this case reinforces the necessity for continued research to better understand this rare disorder and improve diagnostic and therapeutic protocols.
References
1. Wada Takafumi, Kitaguchi Hiroshi, Shindo Katsuro. (2019). Primary angiitis of the central nervous system with cerebral infarction and spinal hemorrhage. Rinsho Shinkeigaku [Clinical neurology], 59(5), 268-273. DOI: 10.5692/clinicalneurol.cn-001288.
2. Salvarani, C., Brown, R. D. Jr., Calamia, K. T., Christianson, T. J. H., Weigand, S. D., Miller, D. V., … Hunder, G. G. (2007). Primary central nervous system vasculitis: analysis of 101 patients. Annals of neurology, 62(5), 442-451. DOI: 10.1002/ana.21226.
3. Hajj-Ali, R. A., & Calabrese, L. H. (2013). Primary angiitis of the central nervous system. Autoimmunity reviews, 12(4), 463-466. DOI: 10.1016/j.autrev.2012.08.005.
4. Birnbaum, J., & Hellmann, D. B. (2009). Primary angiitis of the central nervous system. Archives of neurology, 66(6), 704-709. DOI: 10.1001/archneurol.2009.76.
5. Alrawi, A., Trobe, J. D., Blaivas, M., & Musch, D. C. (1999). Brain biopsy in primary angiitis of the central nervous system. Neurology, 53(4), 858-858. DOI: 10.1212/WNL.53.4.858.
Keywords
1. Primary Angiitis of the Central Nervous System
2. Cerebral Infarction Vasculitis
3. Spinal Hemorrhage Diagnosis
4. Reversible Cerebral Vasoconstriction Syndrome
5. Corticosteroids Therapy Neurology
The synthesis of neurological expertise with advanced imaging and laboratory diagnostics in this article exemplifies the leading-edge work being performed within the field of neurology and provides valuable insights for medical professionals navigating similar challenges.