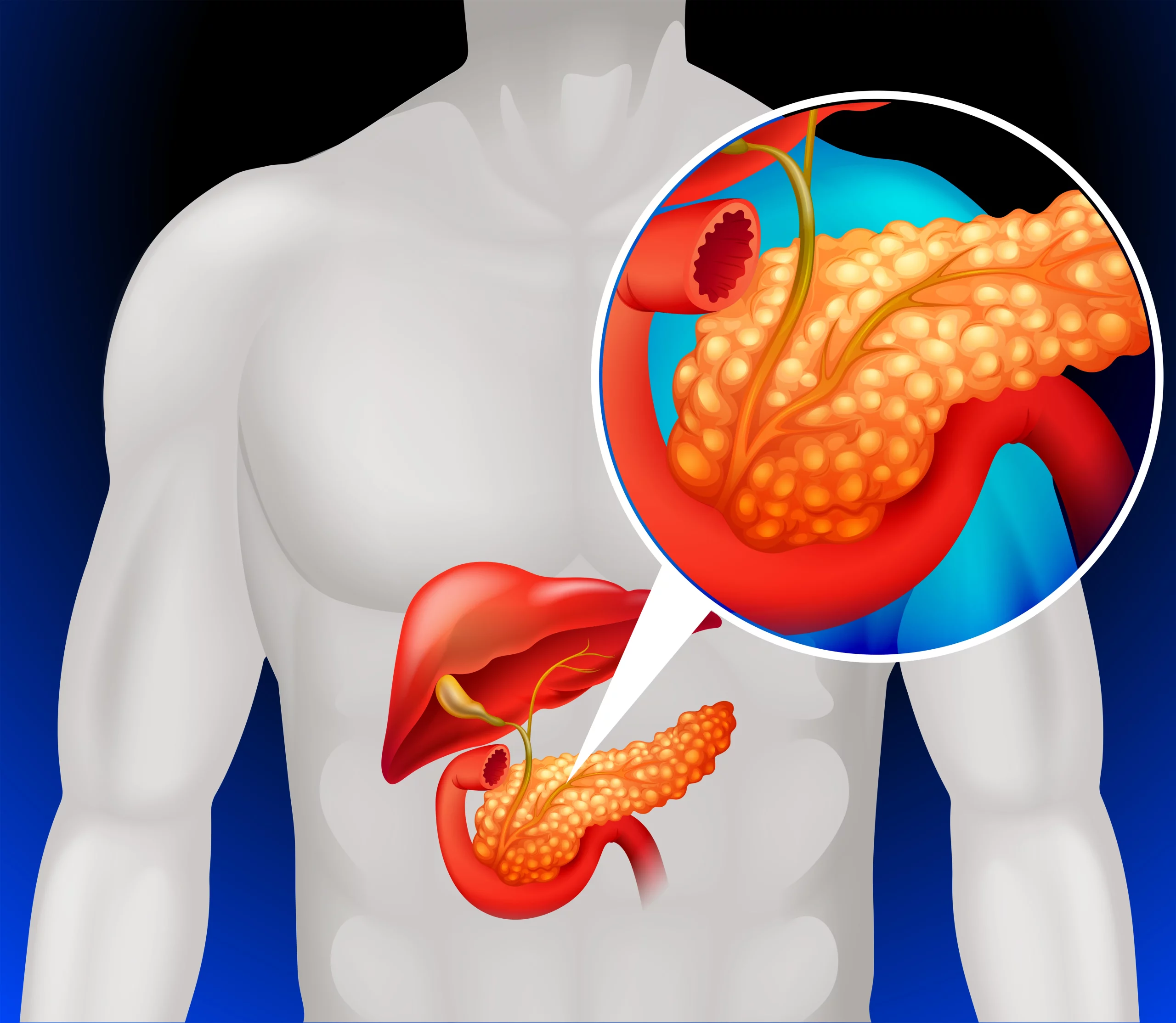
Chronic pancreatitis is a long-term progressive inflammatory disease of the pancreas that leads to permanent breakdown of the structure and function of the pancreas. The pancreas is a large gland behind the stomach which secretes digestive enzymes into the small intestine. It also releases insulin and glucagon into the bloodstream.
When the pancreas becomes inflamed over a long period of time, it can lead to chronic pancreatitis. This inflammation can cause scarring and hardening of the organ, preventing it from functioning correctly. This can lead to a number of symptoms such as abdominal pain, weight loss, and in more severe cases, diabetes.

There are many causes of chronic pancreatitis, but heavy alcohol consumption and smoking are the most common. Other causes include genetic disorders of the pancreas, gallstones, certain autoimmune conditions, and cystic fibrosis. Treatment usually focuses on relieving symptoms and supporting nutritional needs.
Causes of Chronic pancreatitis
Chronic pancreatitis is inflammation of the pancreas that does not heal or improve—it gets worse over time and leads to permanent damage. The following are common causes of chronic pancreatitis:
1. Alcoholism: The majority of chronic pancreatitis cases are due to long-term heavy alcohol consumption. The substances in alcohol can trigger an inflammatory response leading to chronic pancreatitis.
2. Hereditary Disorders of the Pancreas: Hereditary pancreatitis is relatively rare and predisposes individuals to develop chronic pancreatitis at a young age.
3. Autoimmune Diseases: These occur when the body’s immune system attacks the pancreas, leading to chronic inflammation.
4. Cystic Fibrosis: This is a genetic disorder that can damage the pancreas and produce a chronic inflammatory response.
5. Hypercalcemia: High levels of calcium in the blood can cause pancreatitis.
6. Hypertriglyceridemia: High levels of triglycerides in the blood can cause pancreatitis.
7. Certain Medications: Some medicines such as corticosteroids, estrogen, azathioprine, valproate, tetracycline can cause chronic pancreatitis.
8. Repeated Episodes of Acute Pancreatitis: The damage to the pancreas from acute pancreatitis can eventually lead to chronic pancreatitis.
9. Idiopathic Chronic Pancreatitis: In some cases, the cause of chronic pancreatitis is unknown.
These causes lead to multiple bouts of pancreatitis, gradually leading to a situation where the pancreas slowly stops functioning.
Risk Factors of Chronic pancreatitis
Chronic pancreatitis is a long-term inflammation of the pancreas, which leads to permanent damage of this vital organ. There are several risk factors associated with chronic pancreatitis:
1. Alcohol consumption: This is one of the most common causes of chronic pancreatitis. Long term and heavy alcohol consumption can lead to chronic pancreatitis.
2. Smoking: Smoking can increase the risk of pancreatitis, potentially by causing changes in the pancreas that incite inflammation.
3. Cystic Fibrosis: This genetic disorder results in the production of abnormally thick and sticky bodily secretions, including pancreatic juices, which can cause pancreatitis.
4. Hypercalcemia: High levels of calcium in the blood can cause pancreatitis. This can occur due to an overactive thyroid or parathyroid gland.
5. Hypertriglyceridemia: This condition, characterized by high levels of triglycerides in the blood, can also contribute to the development of pancreatitis.
6. Genetic mutations: Some inherited genetic mutations can cause chronic pancreatitis.
7. Autoimmune diseases: Some autoimmune conditions can increase the risk of chronic pancreatitis.
8. Certain medications: Some drugs have been associated with pancreatitis, including certain antibiotics, corticosteroids, and drugs used to treat HIV and hepatitis.
9. Pancreatic duct obstruction: Conditions that obstruct the pancreatic duct, such as pancreatic cancer or gallstones, can lead to chronic pancreatitis.
10. Previous acute pancreatitis: People who have had one or more attacks of acute pancreatitis are more likely to develop chronic pancreatitis.
These risk factors don’t ensure someone will develop chronic pancreatitis, but they significantly increase the risk. If you are concerned about any of these risk factors, you should discuss them with a healthcare provider.
Signs and Symptoms of Chronic pancreatitis
Chronic pancreatitis is a long-standing inflammation of the pancreas that alters its normal structure and functions. Here are some signs and symptoms of chronic pancreatitis:
1. Abdominal Pain: This is often the most prominent symptom. The pain usually occurs in the upper abdomen and may radiate to the back. It might become constant and last for several days.
2. Weight Loss: Unintentional weight loss is often a byproduct of chronic pancreatitis. This is typically due to malabsorption, which is when the pancreas does not produce enough enzymes to break down food.
3. Indigestion: Individuals may suffer from symptoms such as bloating, gas, or a feeling of fullness after a meal.
4. Floating Stools: This is due to poor absorption of fats. The stools may be oily or foul-smelling.
5. Nausea and Vomiting: These symptoms are quite common in chronic pancreatitis, typically exacerbated by eating, particularly high-fat foods.
6. Diarrhea: This can result from the malabsorption of nutrients and fats in the intestines.
7. Diabetes: Chronic pancreatitis can also affect the production of insulin, leading to diabetes. Signs of diabetes include excessive thirst, urination, and fatigue.
8. Jaundice: In some cases, chronic pancreatitis can block the bile ducts, leading to a build-up of bile in the body and resulting in jaundice. Jaundice is recognizable by a yellowing of the skin and eyes.
Remember, these symptoms can also be caused by other medical conditions, so it’s important to consult a healthcare provider for accurate diagnosis and treatment.
Diagnosis Chronic pancreatitis
Chronic pancreatitis is a long-term progressive inflammatory disease of the pancreas that leads to a permanent deterioration of the structure and function of the pancreas. The pancreas is a gland organ that is part of the digestive and endocrine systems. It is located in the abdominal area behind the stomach and produces insulin and other important enzymes and hormones that help break down foods.
This condition happens when the pancreas becomes inflamed over and over again, leading to damage and scarring. This scarring prevents the pancreas from making the right amount of these enzymes and hormones, causing both digestive problems and diabetes.
The most common cause is prolonged alcohol abuse, but also can result from gallstones, cystic fibrosis, high levels of calcium or fats in the blood, certain medications, or autoimmune conditions.
Symptoms often include severe abdominal pain, weight loss, foul-smelling, greasy stools (due to fat malabsorption), and occasionally, individuals might also suffer from diabetes mellitus due to the failure in insulin production.
Treatment often involves managing pain, replacing pancreatic enzymes to aid digestion, dietary changes, and in some severe cases, surgery. It’s also important for patients to avoid alcohol completely to help prevent further pancreatic damage.
Treatment of Chronic pancreatitis
Chronic pancreatitis is a persistent inflammation of the pancreas that results in damage and loss of function over time. Treatment generally targets relief of symptoms, prevention of further damage, and managing complications.
1. Pain Management: Chronic pancreatitis often causes severe abdominal pain. Pain management strategies might include medications, nerve block procedures, or surgery.
2. Enzymes to Improve Digestion: Pancreatic enzyme supplements can help your body break down and process the nutrients in the foods you eat. Pancreatic enzymes are taken with each meal and possibly with snacks.
3. Changes in Diet: A chronic pancreatitis diet is often low in fat and high in carbohydrates. A dietitian can help you put together a meal plan that fits your health goals, food preferences and lifestyle. In some cases, a feeding tube, or nutrition by intravenous (parenteral) means may be necessary.
4. Surgery: In some cases, surgery is required to relieve abdominal pain, to remove a blocked duct or to remove part of the pancreas.
5. Insulin Treatment: Damage to insulin-producing cells in your pancreas from chronic pancreatitis can lead to diabetes. Medications for controlling diabetes, including insulin, may become necessary.
6. Treatment or prevention of complications: Complications can include psuedocysts that may require drainage or removal, infection which may need antibiotics, and nutritional deficiencies which may need vitamins and nutrient supplements.
7. Alcohol Cessation: If the patient’s pancreatitis is caused by alcohol abuse, it’s important they quit drinking alcohol to prevent further damage.

A healthcare provider or specialist can provide detailed information on all potential treatments, their side effects, and their likely success rates. Ongoing and regular check-ups form an essential part of managing the condition. Each patient’s treatment plan may vary as each person’s symptoms and conditions can be unique. It’s crucial to discuss and understand all potential treatment options with a healthcare professional.
Medications commonly used for Chronic pancreatitis
Chronic pancreatitis, an inflammation of the pancreas that does not heal or improve, continues to deteriorate over time, and leads to permanent damage, may require various types of medication for management and treatment. Here are some of the commonly used medications:
1. Pain Medication: Chronic pancreatitis often causes severe abdominal pain. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may help with mild pain. For severe pain, your doctor may prescribe stronger painkillers, such as opioids.
2. Pancreatic Enzymes: Enzyme supplements can help your body break down and process the nutrients in the foods you eat. Pancreatic enzyme supplements are often needed in chronic pancreatitis patients as the pancreas is not producing enough.
3. Insulin: Because chronic pancreatitis can damage the cells that produce insulin, some people may develop diabetes. If that’s the case, insulin or other diabetes medicines may be part of a treatment plan.
4. Antioxidants: Some studies suggest that antioxidant supplementation could have benefits for chronic pancreatitis patients, but more research is needed in this area.
5. Proton Pump Inhibitors (PPIs): These can reduce the production of gastric acid, which may improve the activity of pancreatic enzymes replacement therapy.
6. H2 Blockers: Medications such as ranitidine and famotidine can also reduce acid production, aiding the efficacy of pancreatic enzymes.
Remember, it’s important to consult a healthcare practitioner for a proper diagnosis and treatment approach for chronic pancreatitis.
Please consult with your doctor or healthcare provider for advice tailored to your specific circumstances before making any decisions about your medical care. This advice is intended to be general in nature, and specific causes may require different treatments.
Prevention of Chronic pancreatitis
Chronic pancreatitis is a condition where the pancreas becomes inflamed over a long period of time, leading to permanent damage. It is often linked to alcoholism and smoking, but it can also result from genetic mutations or a blocked pancreatic duct. Here are some ways to help prevent chronic pancreatitis:
1. Limit Alcohol Consumption: Excessive alcohol is one of the primary causes of chronic pancreatitis. To prevent chronic pancreatitis, it is recommended to limit alcohol use to a moderate level or quit altogether.
2. Stop Smoking: Smoking can increase the risk of chronic pancreatitis, as it can exacerbate the damage caused by alcohol on the pancreas.
3. Maintain a Healthy Weight: Obesity can raise the risk of gallstones, a common cause of pancreatitis. Regular physical activity and balanced, healthy eating can help in maintaining an appropriate weight.
4. Balanced Diet: A low-fat, high-protein diet that includes high-fiber foods can aid in preventing chronic pancreatitis. Make sure the diet is rich in fruits, vegetables, whole grains, lean proteins and low-fat dairy.
5. Drink Lots of Water: Staying properly hydrated is essential for overall health and may help prevent the formation of gallstones.
6. Regular Screening: If chronic pancreatitis runs in your family, regular pancreatic screening can be helpful in early detection and prevention.
7. Limit Calcium Intake: In some individuals, high levels of calcium in the blood can cause pancreatitis. It’s important to keep the calcium intake in check.
It’s always best to consult with a healthcare professional to get a personalized advice on prevention strategies based on individual health circumstances.
FAQ’s about Chronic pancreatitis
1. What is Chronic Pancreatitis?
Chronic Pancreatitis is a persistent inflammation of the pancreas, an organ located behind the stomach. This condition is often characterized by abdominal pain and digestive problems due to the pancreas not producing enough digestive enzymes and insulin.
2. What causes Chronic Pancreatitis?
While the exact cause of Chronic Pancreatitis is not always clear, common causes include long-term heavy alcohol use, gallstones, hereditary disorders of the pancreas, cystic fibrosis, high levels of fat in the blood, and certain autoimmune conditions.
3. What are the symptoms of Chronic Pancreatitis?
Symptoms may vary but often include upper abdominal pain, nausea, vomiting, weight loss, diarrhea, and oily or fatty stools. Over time, it can lead to diabetes and digestive problems.
4. How is Chronic Pancreatitis diagnosed?
Diagnosis typically involves a combination of physical examination, medical history, and imaging tests such as a CT scan, MRI, or endoscopic ultrasound. Blood tests can also indicate abnormal levels of pancreatic enzymes.
5. How is Chronic Pancreatitis treated?
The primary goals in treating Chronic Pancreatitis are to relieve pain, manage nutritional and metabolic issues, and treat complications. This might involve pain management, enzyme supplements, dietary changes, insulin therapy, or surgery in severe cases.
6. What is the prognosis for Chronic Pancreatitis?
The prognosis varies depending on the individual and the severity of their condition. In many cases, proper treatment and lifestyle changes can help manage symptoms and prevent further damage to the pancreas.
7. Can Chronic Pancreatitis be prevented?
While not all cases are preventable, individuals can reduce their risk by limiting alcohol consumption, maintaining a healthy diet, exercising regularly, and avoiding smoking.
8. Is Chronic Pancreatitis a life-threatening condition?
Chronic Pancreatitis can lead to serious complications if not treated adequately. These include malnutrition, diabetes, and pancreatic cancer. However, with appropriate management, many people live a full life with the condition.
9. Is Chronic Pancreatitis hereditary?
In some cases, Chronic Pancreatitis can have a genetic component. However, most cases are due to other causes like alcohol abuse or gallstones.
10. Can Chronic Pancreatitis be cured?
While there is no outright cure for Chronic Pancreatitis, the associated symptoms and complications can be managed effectively with the right care and treatment plan.
Useful links
Chronic pancreatitis primarily occurs due to inflammation of the pancreas that does not heal or improve—it gets worse over time and leads to permanent damage. This condition can lead to multiple complications like malnutrition, diabetes, and pancreatic cancer. It’s often linked to heavy alcohol consumption, but other factors can cause it too.
Here are some useful journal links on the topic:
Remember to assess the reliability of the sources by checking their credibilities and availabilities. Furthermore, do consult health professionals for personal health advice.
Complications of Chronic pancreatitis
Chronic pancreatitis, a long-standing inflammation of the pancreas, can lead to several complications. These complications can have substantial effects on the quality of life and may even be life threatening. They include:
1. Pancreatic Exocrine Insufficiency: Chronic pancreatitis can damage the pancreas to the point that it can no longer produce enough of the digestive enzymes it normally creates. This can lead to malnutrition, because the body can’t break down and process nutrients from food.
2. Diabetes: Chronic inflammation of the pancreas may also interfere with insulin production, leading to diabetes.
3. Pseudocysts: The inflammation of the pancreas can lead to fluid and debris accumulation in cyst-like pockets in your pancreas, referred to as pseudocysts. If these rupture, it can cause infection and bleeding.
4. Malnutrition: Damage to the pancreas can mean it produces too few of the enzymes needed to break down food, leading to malnutrition.
5. Pain: Pain is one of the most common complications of chronic pancreatitis. It can be severe and persistent or it may come and go.
6. Pancreatic Cancer: Long-standing inflammation in the pancreas caused by chronic pancreatitis increases the risk of pancreatic cancer.
7. Pancreatic Ascites and Pleural Effusion: These are less common complications, but they occur when pancreatic fluids leak into the abdominal or thoracic cavities.
8. Osteoporosis: Chronic pancreatitis can lead to lower bone density, increasing the risk of fractures.
Always consult with doctors and healthcare professionals to understand, prevent, and manage these complications. Regular visits with them can help diagnose any of these complications early and start appropriate treatments.
Home remedies of Chronic pancreatitis
Chronic pancreatitis is a long-term progressive inflammatory disease of the pancreas that leads to permanent breakdown of the structure and function of the pancreas. The two primary causes of chronic pancreatitis are long-term excessive alcohol intake and gallstone disease. It should be treated under medical supervision.
However, there are a few home remedies that can help manage the symptoms and prevent further complications:
1. A low-fat diet: It’s best to avoid fried and greasy foods. The pancreas plays a crucial role in fat digestion, and a high-fat diet can worsen symptoms.
2. Smaller, more frequent meals: It can be easier on your digestive system to consume five or six small meals a day rather than three large ones.
3. Hydrate regularly: Drink lots of fluids throughout the day, but avoid alcohol as it can exacerbate pancreas inflammation.
4. Quit Smoking: Smoking can intensify symptoms and increase your risk of pancreatic cancer. Seek help to quit if necessary.
5. Maintain a balanced weight: Obesity can worsen pancreatitis, so try to get regular exercise and eat a balanced, nutritious diet to maintain a healthy weight.
6. Limit caffeine: Some people find that caffeine makes their pancreatitis symptoms worse. If you’re one of them, try to cut back on coffee, tea, and other caffeinated beverages.
7. Natural supplements: Certain supplements may help, like vitamins B and E, selenium, magnesium, beta-carotene, and Coenzyme Q10. Always consult a doctor before starting these, as supplements may interfere with other treatments or conditions.
Remember, these remedies support a treatment plan—they don’t replace one. Chronic pancreatitis is a serious condition, so if you or someone else has these symptoms, seek medical attention immediately.