Introduction
In the constantly evolving field of cardiology, alcohol septal ablation (ASA) emerges as a promising treatment for patients with severe left ventricular outflow tract (LVOT) obstruction – a condition that can lead to debilitating symptoms and life-threatening complications. A recent letter published in The Canadian Journal of Cardiology by Dr. Zhehao Dai from the Department of Cardiovascular Medicine at the Graduate School of Medicine, University of Tokyo, sheds light on the implications of this procedure for individuals struggling with complications of cardiomyopathy, particularly hypertrophic cardiomyopathy (HCM). This article unpacks the significance of this study and explores the potential of ASA as a treatment modality.
Understanding LVOT Obstruction
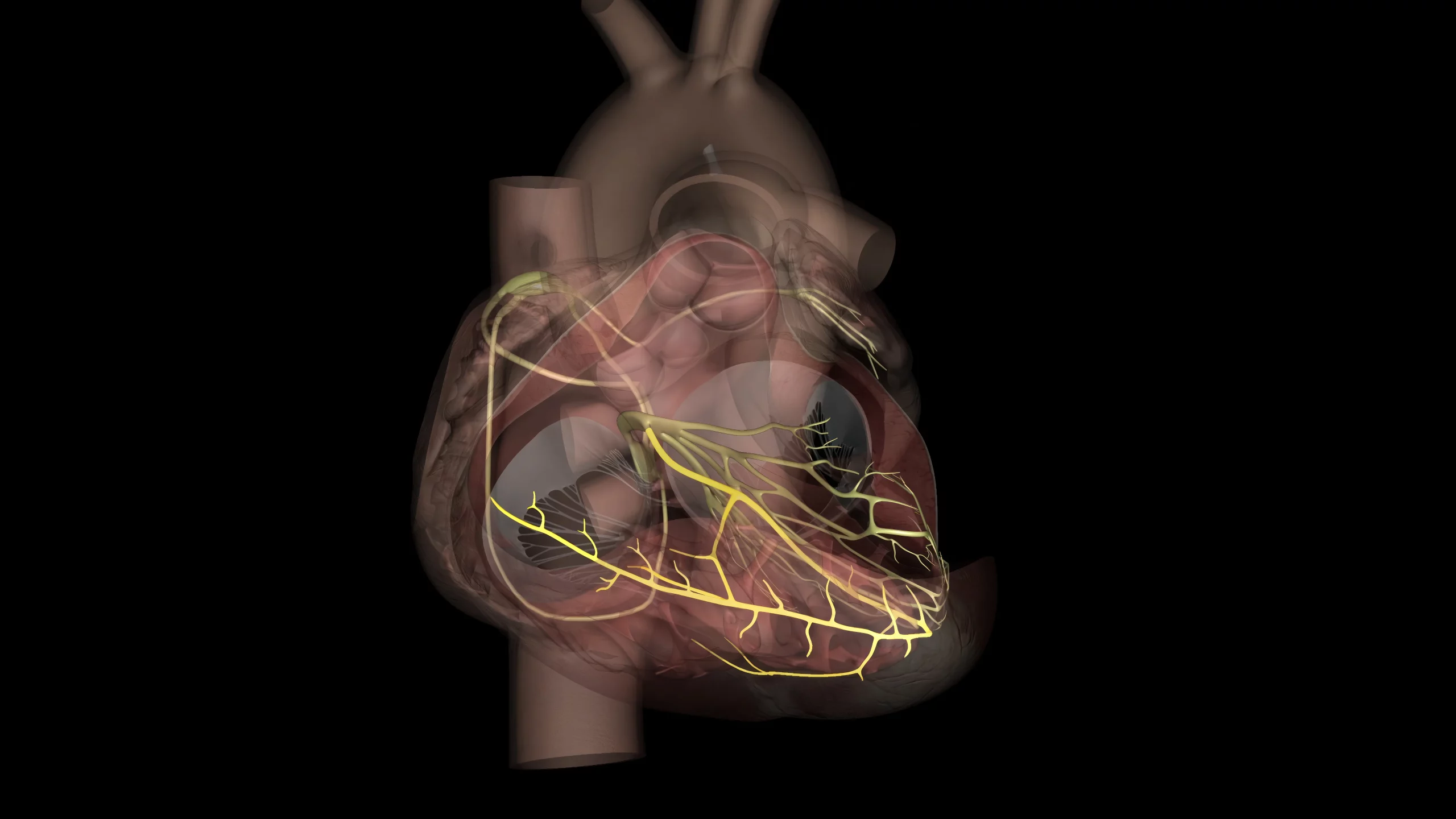
The left ventricular outflow tract is the passage through which blood exits the left ventricle of the heart. Obstruction in this area can be caused by conditions such as hypertrophic cardiomyopathy, resulting in reduced blood flow and increased heart workload. Symptoms of severe LVOT obstruction include shortness of breath, chest pain, and can potentially lead to sudden cardiac death. Current treatments for LVOT obstruction include surgical options like septal myectomy, but they are not without risks and limitations.
Alcohol Septal Ablation as an Alternative
Alcohol septal ablation is a minimally invasive procedure that involves injecting alcohol into the small arteries that supply blood to the part of the heart muscle causing the obstruction, thus reducing its thickness and improving blood flow. ASA has been considered for patients with HCM who are not optimal candidates for surgical intervention. Dai’s correspondence (DOI: 10.1016/j.cjca.2023.07.010) in the January 2024 issue of The Canadian Journal of Cardiology (Can J Cardiol 2024 Jan;40(1):56-56) provides insights into the application of this procedure for individuals with very severe LVOT obstruction.
The Procedure’s Advantages and Risks
ASA offers several advantages including a reduced recovery time compared to surgery, the potential for local anesthesia, and the benefit of being a less invasive technique. Nonetheless, the procedure poses some risks, such as the potential for arrhythmias, heart block requiring a pacemaker, and incomplete symptom relief. It is imperative that patients are carefully selected and thoroughly informed about the benefits and potential complications.
Clinical Outcomes and Treatment Efficacy
While Dai’s letter in the journal does not detail a study but rather offers a perspective on the procedure, it highlights the need for rigorous clinical trials. Previous research has shown variable outcomes, with some patients experiencing significant symptom relief and improved quality of life, while others face the need for additional interventions.
Recommendations for Future Research
The conversation initiated by Dr. Dai underscores the importance of further research to refine the indications for ASA, optimize the technique, and better understand long-term outcomes. Prospective studies comparing ASA with traditional surgical approaches are essential to establishing robust, evidence-based guidelines for treating very severe LVOT obstruction.
Expert Commentary and Conclusion
Renowned cardiologists are cautiously optimistic about the role of ASA in managing severe LVOT obstruction. They stress the necessity for a personalized approach to treatment, recognizing that what works for one patient might not be the best for another. As the medical community continues to advance in its knowledge and techniques, the hope is that ASA could become a standard option for selected patients with this challenging condition.
Keywords
1. Alcohol Septal Ablation
2. LVOT Obstruction Treatment
3. Hypertrophic Cardiomyopathy Therapy
4. Minimally Invasive Cardiac Procedure
5. Heart Muscle Obstruction Solution
References
1. Maron, B. J., & Maron, M. S. (2013). Hypertrophic cardiomyopathy. The Lancet, 381(9862), 242-255. https://doi.org/10.1016/S0140-6736(12)60397-3
2. Sorajja, P., Ommen, S. R., Holmes Jr, D. R., Dearani, J. A., & Gersh, B. J. (2012). Survival after alcohol septal ablation for obstructive hypertrophic cardiomyopathy. Circulation, 126(20), 2374-2380. https://doi.org/10.1161/CIRCULATIONAHA.112.105130
3. Veselka, J., Faber, L., Liebregts, M., Cooper, R., Januska, J., Krejci, J., … & Seggewiss, H. (2017). Indications and contemporary outcomes of alcohol septal ablation in hypertrophic cardiomyopathy. EuroIntervention, 13(8), e949-e956. https://doi.org/10.4244/EIJ-D-17-00584
4. Nishimura, R. A., Seggewiss, H., & Schaff, H. V. (2017). Hypertrophic obstructive cardiomyopathy: Surgical myectomy vs. alcohol septal ablation. Journal of the American College of Cardiology, 70(20), 2522-2529. https://doi.org/10.1016/j.jacc.2017.09.1039
5. Sigwart, U. (2002). Non-surgical myocardial reduction for hypertrophic obstructive cardiomyopathy. The Lancet, 359(9320), 1819-1820. https://doi.org/10.1016/S0140-6736(02)08707-5