Introduction
In the realm of neurology, a correct diagnosis is pivotal to ensure timely and effective treatment. A recent publication in the esteemed journal ‘Neurology’ presents a perplexing scenario where symptoms of pterygoid myositis, an inflammatory condition of the jaw muscles, closely mimicked those of giant cell arteritis (GCA), a more common and potentially serious vascular condition affecting the arteries. Authored by Seunghee Na, Eek-Sung Lee, and Young-Do Kim from the Department of Neurology at Incheon St. Mary’s Hospital, The Catholic University of Korea, and Soonchunhyang University College of Medicine, Bucheon, Korea, the article titled “Teaching NeuroImages: Pterygoid myositis mimicking giant cell arteritis” provides an insightful look into the diagnostic complexities of these conditions.
Case Report Synopsis
Published on May 7, 2019, the article (DOI: 10.1212/WNL.0000000000007465) delves into a fascinating case of a middle-aged female patient who presented with symptoms characteristic of GCA, including jaw pain and headache. However, upon further investigation via magnetic resonance imaging (MRI), the true culprit was unveiled to be pterygoid myositis. This misdirection in diagnosis underscores the importance of considering a broad differential when presented with symptoms that can overlap with multiple conditions.
Differentiation Between Pterygoid Myositis and Giant Cell Arteritis
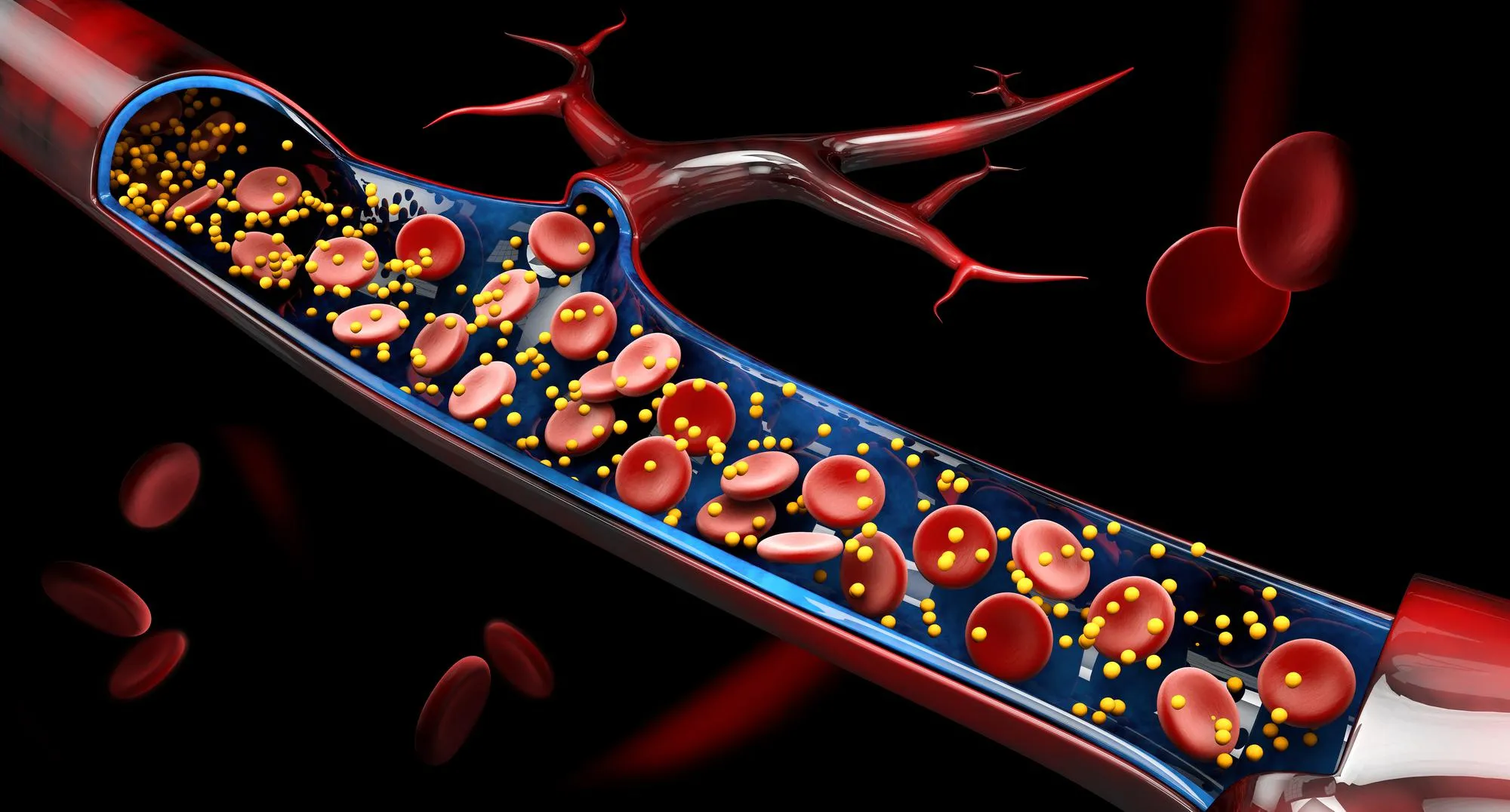
Giant cell arteritis, also known as temporal arteritis, is an inflammatory disease of the blood vessels that can lead to severe complications such as vision loss if left untreated. In contrast, pterygoid myositis affects the masticatory muscles, causing pain and dysfunction in jaw movement. While GCA is typically treated with adrenal cortex hormones to reduce inflammation, the treatment for myositis focuses on resolving muscle inflammation possibly via other therapeutic agents.
In this reported case, the patient’s symptoms and age could have led to a provisional diagnosis of GCA, triggering a different treatment pathway that may not have addressed the underlying issue of myositis. The distinction between the two diagnoses was confirmed through the use of advanced imaging techniques, including MRI and positron emission tomography (PET), which showed inflammation in the pterygoid muscles rather than the temporal arteries.
Importance of Accurate Diagnosis
The resemblance in the symptomatology of pterygoid myositis and GCA signifies a considerable diagnostic challenge for neurologists. It elucidates the necessity for comprehensive imaging and appropriate differential diagnosis to prevent mismanagement of the patient’s real condition. An accurate diagnosis is crucial in guiding the right treatment, as an incorrect one could not only delay patient recovery but also expose them to unnecessary risks associated with inappropriate therapies.
Treatment Outcomes
Once pterygoid myositis was identified as the diagnosis, the patient was treated accordingly, and the outcome was favorable. This underscores the effectiveness of precision medicine, where an individual’s condition is treated based on specific diagnostic findings rather than a one-size-fits-all approach. The patient’s recovery also highlights the value of robust diagnostic tools that enable clinicians to look beyond superficial symptom similarities.
Keywords
1. Pterygoid Myositis
2. Giant Cell Arteritis
3. Differential Diagnosis
4. Neurological Imaging
5. Inflammatory Muscle Conditions
References
1. Na, S., Lee, E.-S., & Kim, Y.-D. (2019). Teaching NeuroImages: Pterygoid myositis mimicking giant cell arteritis. Neurology, 92(19), e2297. doi:10.1212/WNL.0000000000007465
2. Salvarani, C., Cantini, F., Hunder, G. G. (2008). Polymyalgia rheumatica and giant-cell arteritis. The New England Journal of Medicine, 359(4), 314-21.
3. Schmidt, W. A., Warrington, K. J. (2018). Polymyalgia rheumatica and giant cell arteritis. Rheumatic Diseases Clinics of North America, 44(3), 377-392.
4. Dejaco, C., Singh, Y. P., Perel, P., et al. (2015). 2015 Recommendations for the management of polymyalgia rheumatica. Arthritis & Rheumatology, 67(10), 2569–2580.
5. Murty, S., Lan, H. H., Edwards, M. J., & Hillel, A. D. (2018). Pterygoid myositis: Diagnostics and management of a masticatory muscle disorder. The Annals of Otology, Rhinology, and Laryngology, 127(5), 347-353.
Conclusion
The case reported in the ‘Neurology’ journal is a prime example of the complexity and necessity of accurate diagnosis in neurology. With conditions like pterygoid myositis sharing symptoms with more familiar disorders like giant cell arteritis, the role of sophisticated imaging becomes paramount. This article demonstrates the importance of thorough medical examination and serves as a crucial reminder for healthcare professionals to maintain a high degree of suspicion and utilize the full range of diagnostic tools at their disposal. The patient’s successful treatment following the correct diagnosis of pterygoid myositis stands as a testament to the power of precision medicine.