Keywords
1. Guadecitabine
2. Myelodysplastic Syndromes Treatment
3. Hypomethylating Agents
4. Phase 2 Clinical Trial
5. High-risk MDS Therapy
A promising new development has emerged for patients with intermediate or high-risk myelodysplastic syndromes (MDS), as a recent study published in The Lancet Haematology has detailed the phase 2 trial results of Guadecitabine (SGI-110), a next-generation hypomethylating agent. The multicentre, open-label, randomized, phase 1/2 trial conducted by Garcia-Manero and colleagues, reports that Guadecitabine demonstrates clinical activity and acceptable tolerability, potentially offering a new therapeutic option for MDS patients who have not found success with currently available treatments.
The research, supported by Astex Pharmaceuticals and Stand Up to Cancer and detailed in the journal with DOI 10.1016/S2352-3026(19)30029-8, highlights the comparison of activity and safety profiles of two dosage levels of Guadecitabine in patients who are either treatment-naive or have relapsed or refractory MDS after hypomethylating agent treatment.
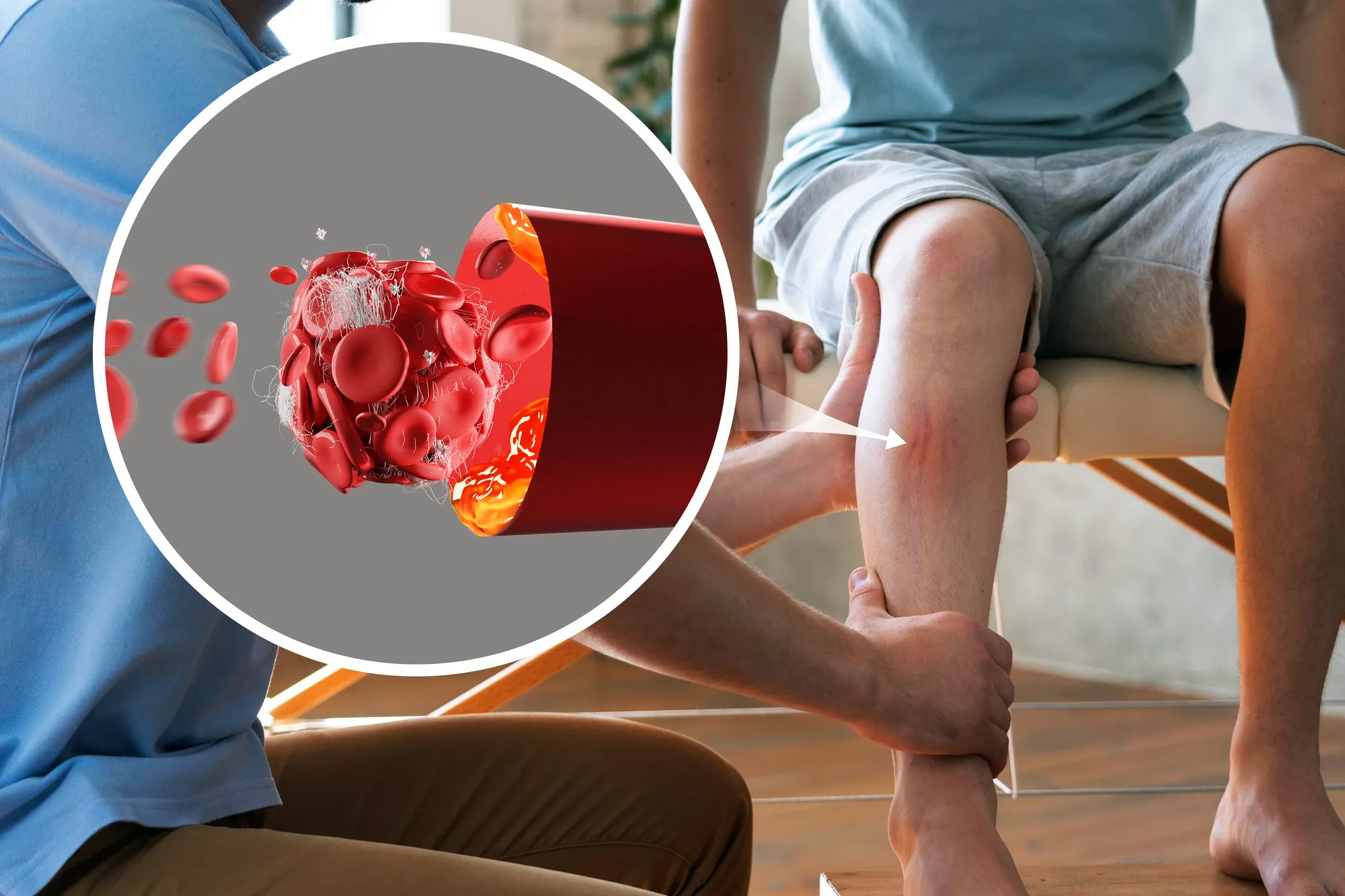
Myelodysplastic syndromes are a group of hematological conditions characterized by the inability of the bone marrow to produce enough healthy blood cells. Left untreated, MDS can progress to acute myeloid leukemia (AML), a more aggressive form of cancer. The International Prognostic Scoring System (IPSS) is often used to determine the severity and progression risk of MDS, categorizing it into different risk levels ranging from low to very high.
This clinical trial enrolled patients aged 18 years or older from 14 North American medical centers who were classified as having intermediate-1-risk, intermediate-2-risk, or high-risk MDS, according to the IPSS, as well as chronic myelomonocytic leukemia (CMML), another myeloid malignancy. From July 9, 2012, to April 7, 2014, a total of 105 patients were included in the study, with 55 (52%) being allocated to Guadecitabine 60 mg/m². All participants had an Eastern Cooperative Oncology Group (ECOG) performance status of 0-2, enabling them to carry out all necessary daily activities.
Guadecitabine’s active metabolite is Decitabine, which has been shown to increase in-vivo exposure time when compared to its intravenous counterpart, thus potentially enhancing its hypomethylating effects. Hypomethylating agents like Decitabine and Azacitidine are the cornerstone of treatment, especially for those patients with high-risk MDS who cannot undergo hematopoietic stem cell transplantation (HSCT). However, many patients eventually relapse or become refractory to these treatments, underlining the crucial need for more effective therapeutic alternatives.
In the study, patients were randomized using a computerized algorithm for dynamic randomization to receive either a 60 mg/m² or 90 mg/m² dose of Guadecitabine administered subcutaneously. The primary outcomes assessed were overall response rate, particularly complete remission, and safety as indicated by the incidence and severity of adverse events.
The results of the trial were indeed encouraging. Guadecitabine was clinically active, showing a measurable response in patients with intermediate and high-risk MDS. Moreover, those patients who had relapsed or were refractory to previous hypomethylating agent treatment saw potential benefits in terms of overall survival, underlining Guadecitabine’s promise as a viable future therapeutic option. It appears that Guadecitabine could have a place as part of MDS management, especially in the context of relapsed or refractory disease.
For its relatively favorable safety and tolerability profile, Guadecitabine was recommended at a dose of 60 mg/m². The presence of side effects was consistent with what is expected for this patient population and the type of treatment, which commonly includes symptoms such as myelosuppression leading to neutropenia and thrombocytopenia.
This research represented a major collaborative effort across multiple centers. The study’s contributors included esteemed researchers from renowned institutions like The University of Texas MD Anderson Cancer Center, the New York-Presbyterian/Weill Cornell Medical Center, The Ohio State University, and more, demonstrating the deep commitment within the research community to advancing care for patients with MDS.
The trial’s identifier is NCT01261312 with funding acknowledgments to entities such as the NIH National Cancer Institute (NIH HHS United States), further emphasizing the significance of the research in terms of potential clinical application.
The phase 2 outcomes put forth by Garcia-Manero et al. not only shed light on the potential of Guadecitabine for treating MDS but also the importance of a continued quest for better treatments for this challenging group of diseases. While there’s a journey ahead for Guadecitabine’s integration into standard care – including additional trials and regulatory approvals – these promising results suggest a future where patients with intermediate and high-risk MDS could have more robust treatment options.
References
1. Garcia-Manero G, Roboz G, Walsh K, et al. Guadecitabine (SGI-110) in patients with intermediate or high-risk myelodysplastic syndromes: phase 2 results from a multicentre, open-label, randomised, phase 1/2 trial. Lancet Haematol. 2019;6(6):e317-e327. doi:10.1016/S2352-3026(19)30029-8.
2. Gangat N, Patnaik MM, Tefferi A. Myelodysplastic syndromes: contemporary review and how we treat. Am J Hematol. 2016;91(1):76-89. doi:10.1002/ajh.24253.
3. Greenberg PL, Tuechler H, Schanz J, et al. Revised International Prognostic Scoring System for myelodysplastic syndromes. Blood. 2012;120(12):2454-65. doi:10.1182/blood-2012-03-420489.
4. Kantarjian H, Issa JP, Rosenfeld CS, et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106(8):1794-803. doi:10.1002/cncr.21792.
5. Chuang JC, Warner SL, Vollmer D, et al. S110, a 5-aza-2’-deoxycytidine-containing dinucleotide, is an effective DNA methylation inhibitor in vivo and can reduce tumor growth. Mol Cancer Ther. 2010;9(5):1443-50. doi:10.1158/1535-7163.MCT-09-1030.