Introduction
Living with chronic thromboembolic disease (CTED) can be a challenging experience, characterized by recurring blood clots in the lungs that can lead to significant exercise intolerance, though it does not show signs of pulmonary hypertension at rest. Traditional treatment has often been limited for CTED patients, providing inadequate relief and quality of life improvements. However, a study published in the International Journal of Cardiology suggests that balloon pulmonary angioplasty (BPA) may offer a ray of hope for those struggling with this affliction.
Understanding CTED
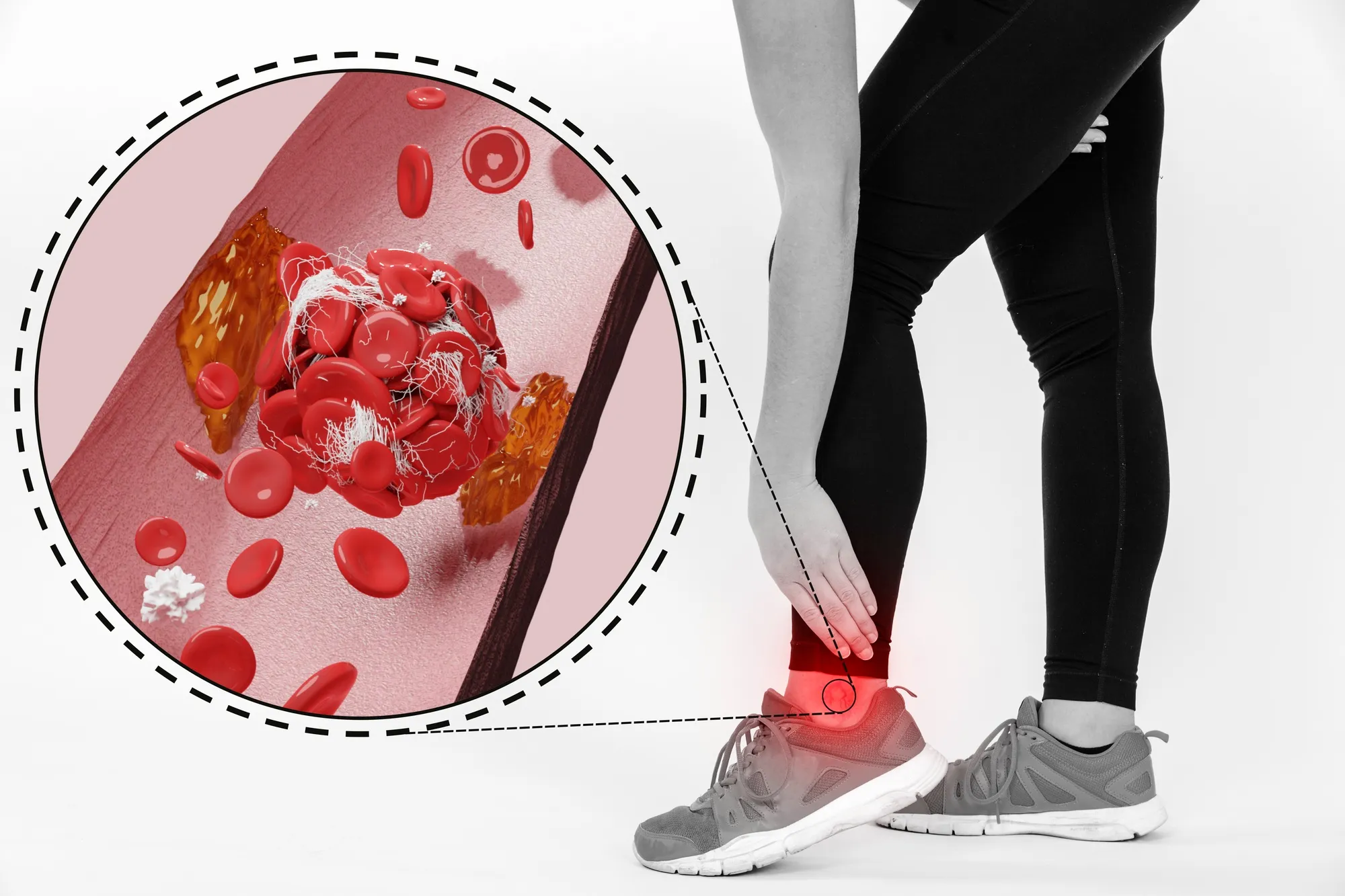
Chronic thromboembolic disease is a condition where blood clots, or thrombi, persist in the pulmonary arteries, leading to obstructed blood flow and reduced oxygen supply to lung tissue. While similar in physiology to chronic thromboembolic pulmonary hypertension (CTEPH), CTED does not elevate pulmonary arterial pressure at rest, thereby distinguishing the two conditions and impacting treatment approaches.
The Efficacy of Balloon Pulmonary Angioplasty
The study, conducted by a research team led by Dr. Takumi T. Inami of the Division of Cardiology, Kyorin University School of Medicine, Tokyo, Japan, investigated the impact of BPA on CTED patients who show no signs of pulmonary hypertension at rest (DOI: 10.1016/j.ijcard.2019.04.080). BPA is a minimally invasive procedure that involves the insertion of a balloon catheter into the pulmonary arteries to expand the vessel and clear obstructions caused by the clots.
Study and Results
In this retrospective study, fifteen patients with CTED were enrolled based on specific inclusion criteria, such as the presence of chronic thromboembolic obstructions verified through ventilation-perfusion scans and pulmonary angiography, functional impairment at WHO functional class II or higher, and a mean pulmonary artery pressure (PAP) of less than 25 mmHg, as measured by right heart catheterization.
Six months post their final BPA session, patients exhibited significant improvements in hemodynamics and a notable increase in their 6-minute walk distance—an indicator of their exercise capacity and overall functional status. Notably, more than half of the participants, who were previously dependent on home oxygen therapy due to hypoxemia, experienced pronounced benefits post-BPA treatment.
Implications for CTED Treatment
This study offers promising evidence that BPA can potentially transform the management of CTED. The observed hemodynamic improvements and increased exercise tolerance hold significant implications for improving the quality of life for patients suffering from this chronically debilitating condition.
Limitations and Future Directions
While the findings point towards the effectiveness of BPA in CTED, the researchers acknowledge the limitations of their study, including its small sample size and retrospective nature. The study’s lead authors, Inami & Kataoka, advocate for prospective, larger randomized clinical trials to validate and expand upon the treatment strategy delineated by their research.
Expert Commentary
Experts in the field concur with the study’s recommendation for further research. Pulmonary specialists and cardiologists alike are optimistic that subsequent trials will not only corroborate these initial positive results but will also refine treatment protocols, improve patient selection criteria, and enhance the overall therapeutic approach to CTED.
Patient Perspectives
Patients who have undergone BPA for CTED report significantly improved quality of life, with many experiencing less fatigue, greater exercise tolerance, and a reduced need for supplemental oxygen. These anecdotal reports align with the scientific evidence presented by the study, adding a human dimension to the statistical improvements described.
Conclusion
The Inami and Kataoka study marks a pivotal development in the management of CTED. It underscores the potential of BPA to offer symptomatic relief and suggests a possible shift towards more active treatment protocols for those with CTED. With ongoing research, continued advancements in the field are anticipated, which could ultimately redefine the standard of care for patients with chronic thromboembolic disease without pulmonary hypertension at rest.
References
1. Inami, T., Kataoka, M., Kikuchi, H., Goda, A., & Satoh, T. (2019). Balloon pulmonary angioplasty for symptomatic chronic thromboembolic disease without pulmonary hypertension at rest. International Journal of Cardiology, 289, 116-118. DOI: 10.1016/j.ijcard.2019.04.080
2. Jenkins, D. et al. (2013). Diagnosis and management of chronic thromboembolic pulmonary hypertension: Statements from the British Thoracic Society Standards of Care Committee Pulmonary Embolism Guideline Development Group. Thorax, 68(Suppl 2), ii1-ii58. DOI: 10.1136/thoraxjnl-2013-203600
3. Lang, I.M. et al. (2017). Balloon pulmonary angioplasty in chronic thromboembolic pulmonary hypertension. European Respiratory Journal, 49(6). DOI: 10.1183/13993003.01532-2016
4. Madani, M.M. et al. (2016). Chronic Thromboembolic Pulmonary Hypertension: Operative Management. European Journal of Cardio-Thoracic Surgery, 49(4), 1138-1144. DOI: 10.1093/ejcts/ezv405
5. Mayer, E. et al. (2011). Surgical management and outcome of patients with chronic thromboembolic pulmonary hypertension: Results from an international prospective registry. Journal of Thoracic and Cardiovascular Surgery, 141(3), 702-710. DOI: 10.1016/j.jtcvs.2010.11.024
Keywords
1. Chronic Thromboembolic Disease Treatment
2. Balloon Pulmonary Angioplasty
3. Exercise Tolerance Improvement
4. Pulmonary Artery Obstruction Intervention
5. Non-Hypertensive CTED Management