Abstract
A recent study, published in the Annals of Clinical Microbiology and Antimicrobials, has shed light on the genomic diversity of β-lactamase producing Pseudomonas aeruginosa in Iran, highlighting the serious impact that global high-risk clones are exerting on health systems. This cross-sectional study assessed the antibiotic susceptibility and genomic relationships of 155 P. aeruginosa isolates, uncovering that high-risk clones responsible for hospital-acquired infections are now widespread in the region, necessitating immediate containment strategies.
Introduction
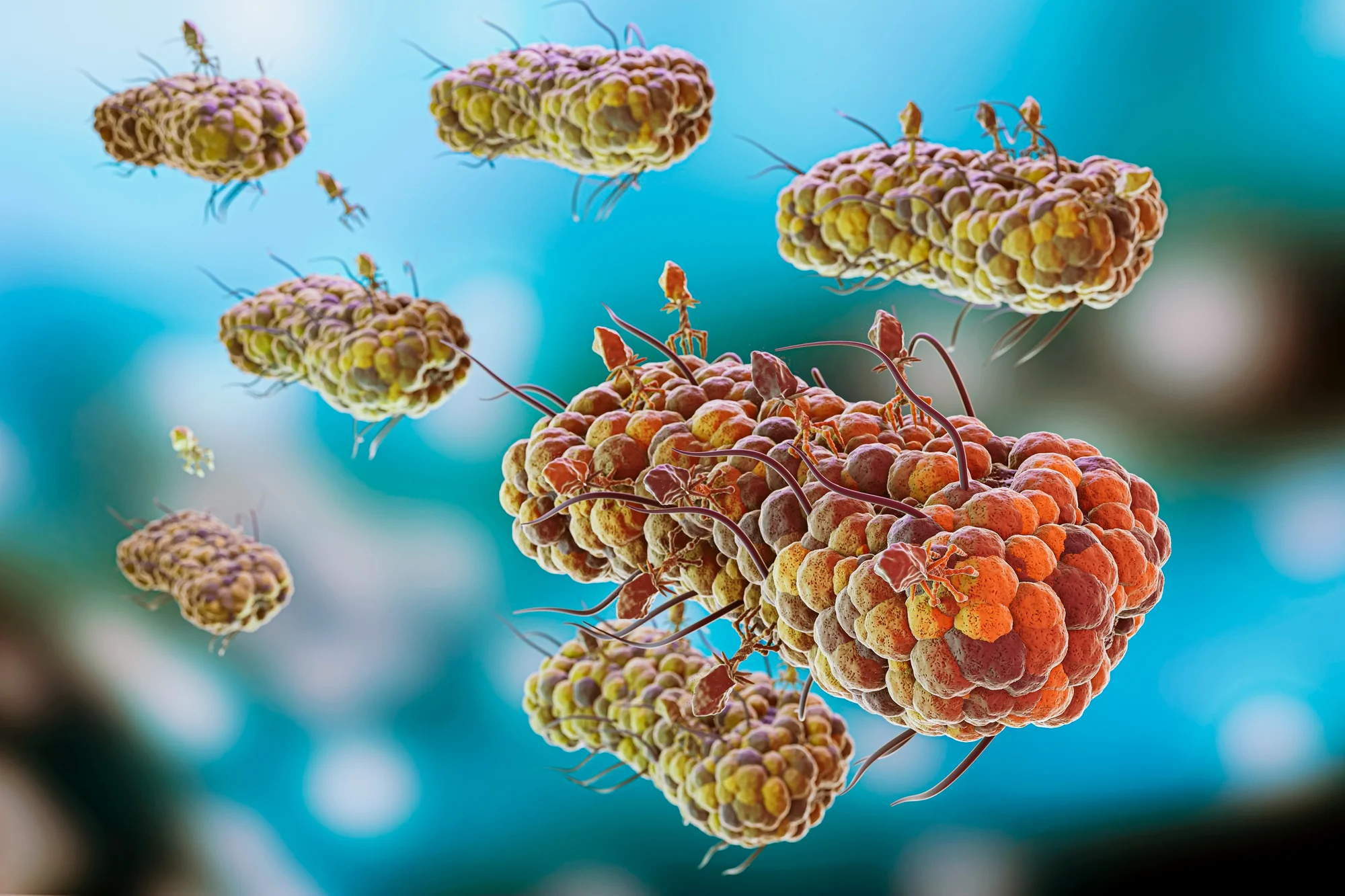
In the battle against microbial resistance, the name Pseudomonas aeruginosa rings alarm bells in healthcare settings worldwide. Armed with the ability to wield β-lactamases, enzymes that confer resistance to β-lactam antibiotics, this pathogen has become a formidable adversary in hospital-acquired infections. The escalation of multidrug-resistant (MDR) strains has resulted in prolonged hospitalization, skyrocketing treatment costs, and a concerning upsurge in mortality rates.
A study published on January 18, 2024, in the Annals of Clinical Microbiology and Antimicrobials by Nazila N. Ahmadi and colleagues from various respected Iranian universities, has brought to light the concerning prevalence and diversity of β-lactamase producing strains of P. aeruginosa in Iran. This elaboration aims to dissect their findings, discuss the global implications, and consider the steps that must be taken to curb the tide of this microbial threat.
Methodology
The study by Ahmadi et al. was a cross-sectional investigation of 155 non-repetitive P. aeruginosa isolates collected from different medical centers across Iran. Antibiotic susceptibility was determined using phenotypic and genotypic methods, while clonal relationships were explored through multi-locus sequence typing (MLST) and repetitive extragenic palindromic PCR (REP-PCR).
Results
The findings revealed that colistin remains the most effective antibiotic against P. aeruginosa, with a susceptibility rate of 94.9%. Narrow spectrum β-lactamases, including SHV, PER, OXA-1, and TEM, were identified with varying frequencies, while 18% of isolates were found to be carbapenemase-producers—the highest frequencies being IMP and NDM enzymes. MLST analysis pinpointed several sequence types, such as ST244, ST664, ST235, and ST357, that were prevalent among carbapenem-resistant isolates. REP-PCR analysis indicated significant genomic diversity, identifying the propagation of ST235 as a key contributor to the multidrug resistance pattern in P. aeruginosa.
Discussion
The disclosed genomic diversity and prevalence of high-risk P. aeruginosa clones in Iran ring the alarm for an imminent health crisis. ST235, in particular, has been identified as a significant threat due to its role in disseminating MDR patterns. These trends concur with global observations where certain high-risk clones, such as ST235, ST111, and ST175, have been singled out for their contribution to the spread of resistance. This scenario complicates infection control and treatment, highlighting the need for robust surveillance systems and concerted regional and international efforts in microbial containment.
Policy Implications
Ahmadi et al.’s study is a wake-up call to health authorities for framing stringent infection control policies and antimicrobial stewardship programs. It becomes imperative to bolster sanitation, adopt effective antimicrobial regimens, and invest in rapid diagnostic technologies. Additionally, the fostering of international collaboration in research, surveillance, and control strategies must be prioritized to tackle the global dissemination of high-risk clones.
Conclusion
The study by Ahmadi and colleagues provides a crucial snapshot of the β-lactamase producing P. aeruginosa landscape in Iranian hospitals. Their work emphasizes the urgent need for immediate and structured action to manage the spread of MDR bacteria. It is a stark reminder that in the arms race against P. aeruginosa, our armamentarium is weakening, and without sustained and concerted efforts, we risk losing ground in our fight against bacterial infections.
DOI: 10.1186/s12941-024-00668-5
References
1. Rossolini GM, Mantengoli E, “Treatment and control of severe infections caused by multiresistant Pseudomonas aeruginosa,” Clin Microbiol Infect, 2005;11:17–32.
2. Glen KA, Lamont IL, “β-lactam Resistance in Pseudomonas aeruginosa: Current Status, Future Prospects,” Pathogens, 2021; PMC8706265.
3. Poole K, “Pseudomonas aeruginosa: Resistance to the Max,” Front. Microbiol, 2011; p. 65.
4. Oliver A et al., “The increasing threat of Pseudomonas aeruginosa high-risk clones,” Drug Resist Updat, 2015;21–22:41–59.
5. Wright LL et al., “Dominance of international ‘high-risk clones’ among metallo-β-lactamase-producing Pseudomonas aeruginosa in the UK,” J Antimicrob Chemother, 2015;70:103–10.
Keywords
1. Pseudomonas aeruginosa
2. β-lactamase resistance
3. High-risk clones
4. Antimicrobial resistance
5. Hospital-acquired infections