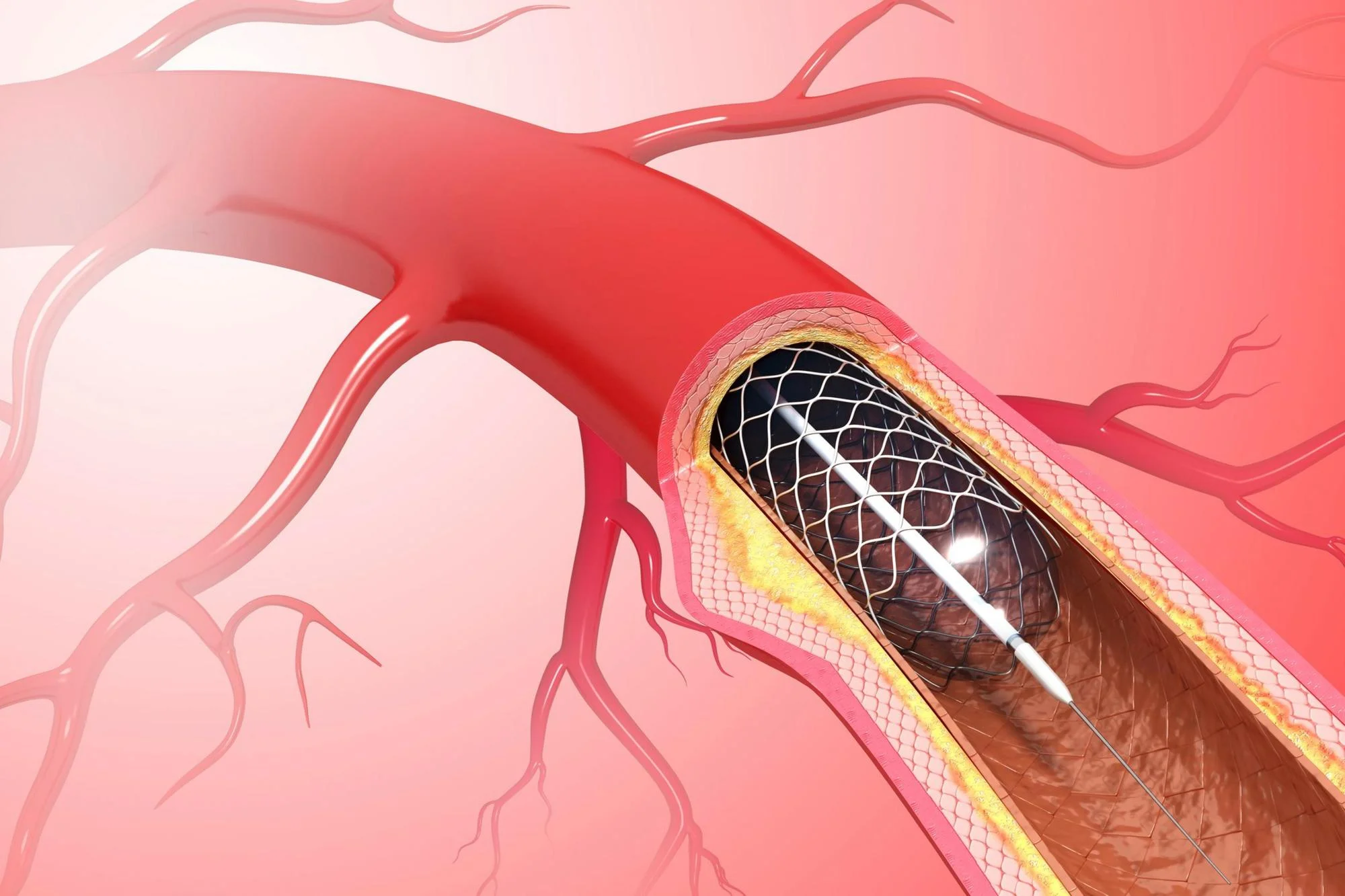
Following the implantation of a drug-eluting stent (DES), patients at high bleeding risk (HBR) face a complex recovery period marked by careful management to minimize adverse outcomes. In a ground-breaking study published on January 12, 2024, in the Hellenic Journal of Cardiology, researchers uncovered significant sex-based differences in ischemic cardiovascular events and bleeding outcomes among HBR patients. This new evidence calls for a more personalized approach to post-stent care, specifically tailored to address these disparities.
The study, titled “Sex-based differences in ischemic cardiovascular and bleeding outcomes following implantation of drug-eliting stent in patients at high bleeding risk,” emerges from a comprehensive analysis of patient data in Taiwan (Lin et al., 2024). The researchers harnessed the National Health Insurance Research Database to examine a cohort of patients who showed HBR features as defined by the Academic Research Consortium. They included those who received DES implantation from January 1, 2007, to December 31, 2017.
Lin and colleagues utilized a rigorous propensity score matching method to compare 3,981 pairs of male and female patients with similar clinical cardiovascular risks. The main goal was to dissect the nuanced yet critical differences between sexes in the context of post-DES implantation outcomes.
Discovering the Gap
The researchers were meticulous in their approach, employing a competing risk model to identify the risk of adverse ischemic events — which included cardiac death, nonfatal myocardial infarction, and ischemic stroke — and any bleeding events. Noncardiac death presented as a competing risk in this intricate equation.
Over the 5-year follow-up window, the findings were striking: males demonstrated a consistent yet marginally increased risk in composite ischemic events, with an incidence rate of 44.09 per 1,000 person-years (95% CI: 40.25-48.30), compared to the rate of 40.18 per 1,000 person-years (95% CI: 36.51-44.23) observed in females.
However, when it came to bleeding events, the sexes were almost at par. Males saw an incidence rate of 42.55 per 1,000 person-years (95% CI: 38.79-46.68), while females experienced 42.35 per 1,000 person-years (95% CI: 38.57-46.51). Even after adjusting for clinical variables, males displayed a modestly elevated risk of ischemic outcomes with an adjusted subdistribution hazard ratio (SHR) of 1.15 (1.00-1.31, p=0.045), but an equivalent risk of bleeding events at an adjusted SHR of 1.00 (0.88-1.15, p=0.946).
Implications for Personalized Care
This insightful research contributes significantly to the ongoing conversation regarding personalized medicine, particularly in cardiology. The authors, spearheaded by Lin Chao-Feng of MacKay Medical College and colleagues from various prestigious institutions, encourage the medical community to deliberate on the sex-based differences elucidated by their study.
Indeed, males’ increased risk of ischemic outcomes signifies a potential need for more aggressive or extended ischemic preventive strategies, simultaneous with measures to maintain bleeding risk management. These findings suggest that while DAPT adherence is critical for HBR patients regardless of sex, additional considerations may need to be made for male patients to reduce their higher propensity for ischemic events.
Recommendations for Clinical Practice
To translate these findings into clinical practice, healthcare providers might need to:
1. Re-evaluate the risk-benefit ratio of DAPT duration on a sex-specific basis.
2. Consider closer monitoring of male patients post-DES implantation for early detection of ischemic events.
3. Explore sex-specific genetic, hormonal, or lifestyle factors that could contribute to the risk disparities.
Future Research Directions
Lin et al.’s research opens the door for further studies into the mechanisms behind these sex-based differences. Investigations could delve into the interaction of sex hormones with platelet function and endothelial healing post-DES implantation, or examine the role of genetics in susceptibility to ischemic events.
Moreover, global validation of these findings in different populations and healthcare settings remains paramount to establish comprehensive, universal care guidelines that account for these sex-specific nuances.
Reflecting on the Study’s Strengths and Limitations
The robust methodology and extensive dataset of the study by Lin et al. strengthen the validity of the results. Propensity score matching, in particular, helps to reduce the impact of confounding variables, providing a more authentic comparison between male and female patients.
However, as with all research, certain limitations must be acknowledged. The study’s observational nature cannot establish causality, and its reliance on a Taiwanese database may limit the generalizability of the results to other ethnic or racial populations.
Conclusion
The research by Lin et al. (2024) serves as a clarion call for the nuanced consideration of sex-specific differences in the management of HBR patients post-DES implantation. As the authors rightly state, “Of the HBR population, males had an increased risk of ischemic outcomes but a similar risk of bleeding compared with females following DES implantation” (Lin et al., 2024). This pivotal research propels the medical field toward an era of more personalized, gender-sensitive cardiovascular care, promising improved outcomes for patients worldwide.
DOI and References:
DOI: 10.1016/j.hjc.2024.01.001
Lin Chao-Feng, Tsai Chia-Ling, Chang Ya-Hui, Lin Dai-Yi, and Chien Li-Nien. “Sex-based differences in ischemic cardiovascular and bleeding outcomes following implantation of drug-eluting stent in patients at high bleeding risk.” Hellenic Journal of Cardiology (2024).
Keywords
1. Drug-eluting stent outcomes
2. High bleeding risk patients
3. Sex-based differences in cardiology
4. Dual antiplatelet therapy adherence
5. Ischemic events post-stent implantation
By incorporating these keywords, the article is positioned to effectively reach healthcare professionals and patients alike, disseminating crucial insights about sex-specific risk profiles in post-stent care that can influence treatment plans and improve patient outcomes.