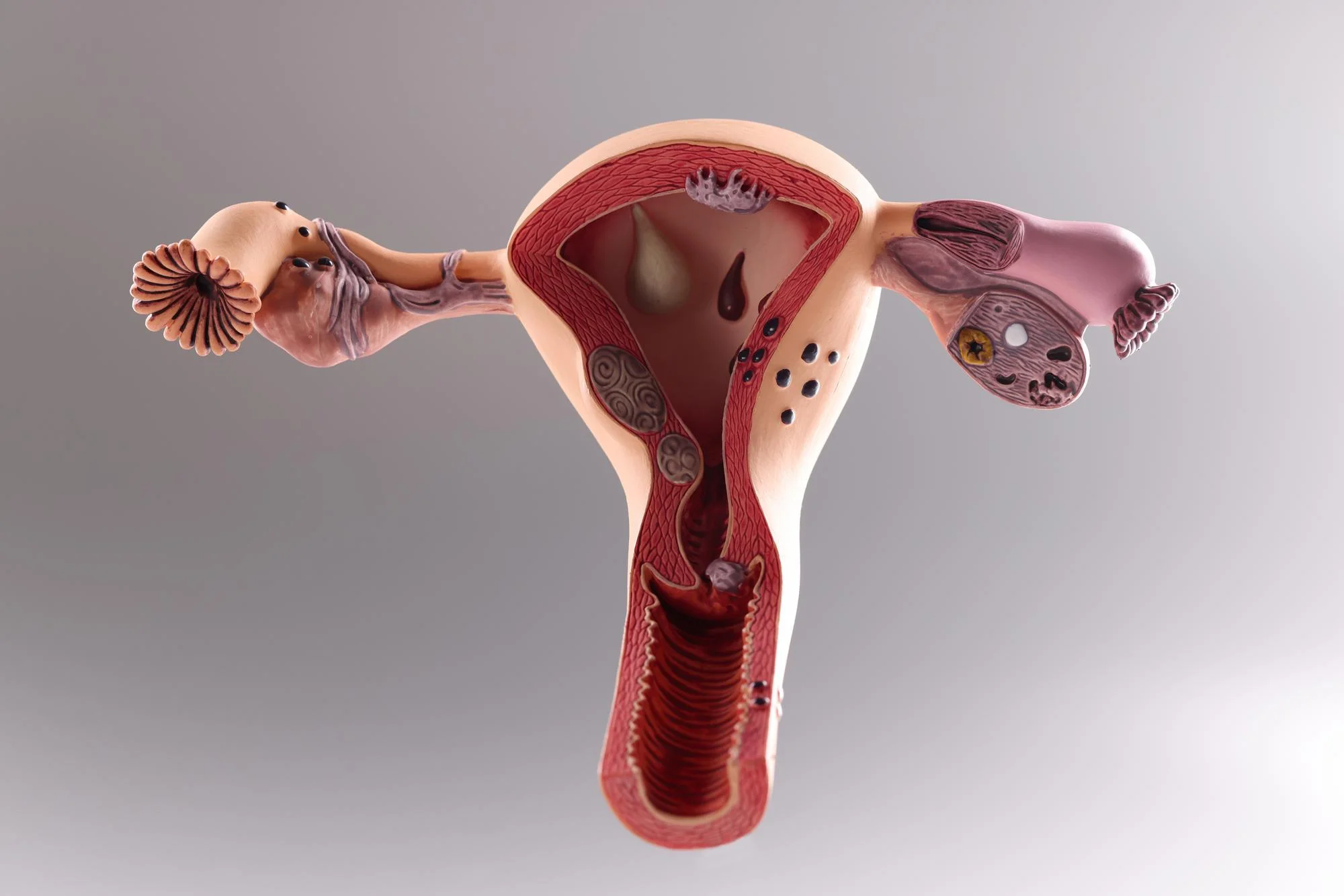
Womb cancer, also known as uterine cancer or endometrial cancer, is a common type of cancer that begins in the layer of cells that form the lining (endometrium) of the uterus.
Most womb cancers are endometrial carcinomas which start in the cells of the endometrium. However, there are other types as well, which include uterine sarcoma that begin in the muscle or other tissues in the uterus.
The exact cause of womb cancer isn’t known, but certain factors can increase a woman’s chance of getting it, like age (most cases are diagnosed in women aged 40-74), increased levels of estrogen, being overweight or obese, having diabetes, or having gone through the menopause.

Symptoms of womb cancer can include abnormal bleeding, such as bleeding outside of your normal menstrual cycle, bleeding after menopause, heavier periods than you normally have, and watery or blood-tinged discharge from your vagina.
The treatment for womb cancer depends on how advanced it is. This can range from surgery, which may involve the removal of the uterus (hysterectomy) to radiation therapy and chemotherapy. Early detection of this cancer significantly increases the chance of successful treatment. So, it’s very important to have regular gynecological check-ups and to consult a doctor if you notice any signs or symptoms. It’s also important to lead a healthy lifestyle to lower risks of not just womb cancer, but other types of cancers and diseases as well.
Causes of Womb (uterus) cancer
Uterus (or womb) cancer, also known as endometrial cancer, is typically caused by a variety of factors. However, it’s important to remember that having one or many of the risk factors does not inherently mean one will get the disease.
1. Age: The risk of developing endometrial cancer increases with age. Most cases are diagnosed in women over the age of 50.
2. Hormone Levels: The balance of hormones in a woman’s body plays an important role in the development of endometrial cancer. Estrogen helps the lining (endometrium) of the womb grow and thicken. Progesterone gets the lining ready to receive and nurture a fertilized egg. If there’s too much estrogen and not enough progesterone, the lining of the womb can grow too much and become cancerous.
3. Obesity: Fat tissue can increase levels of estrogen, which could increase the risk of endometrial cancer.
4. Genetics: Some inherited genetic syndromes, like Lynch syndrome, can increase the risk of endometrial cancer.
5. Other Health Conditions: Conditions like polycystic ovary syndrome (PCOS), diabetes, and hypertension can also increase the risk.
6. Use of Tamoxifen: Women who have taken tamoxifen for breast cancer treatment or to lower their risk of breast cancer have an increased risk of endometrial cancer.
7. Reproductive History: Conditions associated with increased exposure to estrogen, such as beginning periods at an early age, menopause at a later age, not having children, infertility, or having fewer menstrual cycles due to irregular periods or fewer pregnancies also carry an increased risk.
Remember, the presence of these factors does not guarantee the development of uterus cancer, just as the absence of these factors does not ensure one will not develop the disease. It is always important to get regular check-ups and discuss any changes you notice in your body with your doctor.
Risk Factors of Womb (uterus) cancer
Womb or uterus cancer, also known as endometrial cancer, has several risk factors associated with it. It’s always important to remember that having one or more of these risk factors doesn’t necessarily mean you’ll develop the disease, but it may increase your risk. Here are the most common risk factors:
1. Age: Uterus cancer risk increases with age. Most cases are diagnosed in women who are over 50 years of age and have gone through menopause.
2. Obesity: Overweight and obesity are significant risk factors because fat cells produce excess estrogen, which can stimulate the growth of the endometrial lining and increase your risk of developing endometrial cancer.
3. Hormone Therapy for Breast Cancer: Women who take estrogen alone without a progesterone supplement for hormone therapy during menopause have an increased risk of endometrial cancer.
4. Tamoxifen: This is a drug used to prevent and treat breast cancer, but it can also increase the risk of endometrial cancer.
5. Family history: Women who have a family history of endometrial cancer, particularly a mother, sister, or daughter, are at increased risk.
6. Genetics: Women with inherited colon cancer syndrome, also known as Lynch syndrome, are at significantly increased risk.
7. Diabetes: Women with diabetes are at higher risk than women without diabetes.
8. Polycystic Ovarian Syndrome: Women with this condition often have irregular periods, obesity, and high levels of insulin and male hormones. All of these factors raise the risk of endometrial cancer.
9. Irregular periods or infertility: Women who have never had children, have irregular periods, or who start their periods before age 12 or have menopause after age 55, have more menstrual cycles and are exposed to higher levels of natural oestrogen, which can increase risk.
10. Endometrial hyperplasia: This is a condition in which the endometrium (the lining of the uterus) becomes too thick. It’s not a type of cancer, but sometimes it can develop into cancer.
Remember that most people with these risk factors never develop womb or uterus cancer. However, if you believe you may be at risk, you should discuss this with your doctor. They may be able to suggest lifestyle changes to help reduce your risk or may recommend regular screenings.
Signs and Symptoms of Womb (uterus) cancer
Uterine (womb) cancer symptoms can vary widely, and some women do not experience significant symptoms until the cancer has progressed. However, it’s important to be aware of the potential signs and symptoms, which may include:
1. Abnormal Vaginal Bleeding: The most common sign is unusual vaginal bleeding, typically post menopause. It can start as a watery, blood-streaked flow and gradually contains more blood. Women who haven’t reached menopause might have heavier menstruation or unpredictable periods.
2. Unusual Vaginal Discharge: Some women may experience a watery or blood-tinged discharge unrelated to their periods.
3. Pain During Intercourse: Sex might become painful in the advanced stages of this cancer.
4. Pelvic Pain: A less common symptom is pain in the lower abdomen or pelvic area.
5. Difficulty or Pain When Urinating: This might be a symptom especially if the cancer has progressed to an advanced stage.
6. Unintentional Weight Loss: This is rare but could potentially occur in advanced cases.
It’s essential to be aware that these symptoms can also be associated with many conditions other than cancer. But if you’re experiencing any of these symptoms persistently, it’s crucial to discuss them with your doctor so they can identify any potential issues and treat them appropriately. The earlier a diagnosis is made, the better the outcome is likely to be.
Diagnosis Womb (uterus) cancer
Womb or uterus cancer refers to any type of cancer that emerges from the tissue of the uterus. It can refer to several types of cancer, with endometrial cancer (cancer of the lining of the uterus, or endometrium) being the most common form.
Signs and symptoms of womb cancer can vary but often include abnormal vaginal bleeding, pelvic pain, pain during intercourse, and an enlarged uterus.
The exact cause of uterine cancer is unknown, though certain factors can increase the risk of developing the disease. These include age, obesity, certain inherited colon cancer syndromes, use of tamoxifen for breast cancer treatment, never having been pregnant, late menopause, and estrogen replacement therapy without progesterone.
Womb cancer diagnosis typically involves a series of tests, starting with a general physical examination. This could be followed by blood tests, a transvaginal ultrasound scan, or a hysteroscopy. If the doctor suspects cancer, a biopsy may be taken, which is the most reliable way to confirm the diagnosis. Stages of the disease range from stage I (cancer only in the uterus) to stage IV (cancer has spread to other parts of the body).
Doctors typically recommend surgery (like hysterectomy, which involves removing the uterus), radiation therapy, chemotherapy, hormone therapy, or a combination of these, depending on the type and stage of the cancer.
Treatment of Womb (uterus) cancer
The treatment for womb or uterus cancer largely depends on the size of the tumor and how far it has spread. Here are some common methods for treatment:
1. Surgery: Hysterectomy, where the uterus is removed, is often the first step. Sometimes, the fallopian tubes and ovaries are also removed. If the cancer has spread, more tissues may be removed such as the lymph nodes to prevent further spread.
2. Radiation therapy: High-energy X-rays are used to kill off cancer cells. Radiation therapy is either given externally by a machine, or internally by placing a small radioactive device inside your body.
3. Chemotherapy: This systemic treatment uses drugs to kill cancer cells. These medications may be taken orally or injected into the body.
4. Hormone therapy: For some types of uterus cancer, hormone treatment might be effective: progesterone can prevent cancer cells from growing, while aromatase inhibitors can reduce the amount of estrogen in the body, which might help slow down or stop the growth of cancer cells.
5. Targeted therapy: These therapies specifically target the cancer’s specific genes, proteins, or the tissue environment that contributes to cancer growth and survival.
6. Immunotherapy: This treatment can boost or restore the ability of the immune system to fight cancer.
Remember, the specifics of treatment are individualized and depend on the stage of the cancer, the patient’s overall health, and their personal preferences. It’s crucial to have a discussion with the patient’s doctor to achieve the best possible outcome. It’s also beneficial to have a support system during treatment, handle possible side effects, and maintain physical health as much as possible.
Medications commonly used for Womb (uterus) cancer
Treatment for uterine (womb) cancer often involves a combination of surgery, radiation therapy, and chemotherapy. Common types of medications used to treat this cancer are primarily chemotherapeutic agents.
These may include:
1. Paclitaxel (Taxol): This medication stops cancer cells from multiplying and has shown effect in treating uterine cancer.
2. Carboplatin: This platinum-containing compound has shown efficacy in numerous cancer types including uterine cancer. It stops cancer cells from dividing and growing.
3. Doxorubicin: Also known as Adriamycin, Doxorubicin slows or stops the growth of cancer cells.
4. Cisplatin: Another platinum-based chemotherapy drug. It interferes with DNA in cancer cells, preventing them from dividing and growing.
5. Ifosfamide (Ifex): An alkylating agent that works by damaging the DNA in cancer cells to interfere with their ability to replicate.
6. Docetaxel (Taxotere): This medication interferes with the cancer cells’ ability to divide and grow.
7. Gemcitabine (Gemzar): This drug is a cytotoxic which kills cancer cells and prevents them from dividing and growing.
Hormone therapy using progesterone is also sometimes used, particularly in later stages of the disease or when other treatments are not suitable.
Always remember that your healthcare provider will choose the best treatment options based on many factors, including the type and stage of cancer, your overall health, and potential side effects.
Prevention of Womb (uterus) cancer
Uterus (also known as womb) cancer can be prevented or its risk can be reduced by implementing certain lifestyle changes and taking necessary precautions. Here’s how:
1. Maintain a healthy weight: Obesity increases the risk of uterus cancer. Therefore, balancing caloric intake and regular exercise is essential for maintaining a healthy weight.
2. Regular exercise: Regular physical activity can lower your risk of developing uterus cancer. It could be anything from walking, swimming, jogging to cycling.

3. Eat healthy: A diet rich in fruits, vegetables, and whole grains can help prevent various types of cancers.
4. Consider birth control pills: Women who use oral contraceptives have a lower risk of womb cancer. However, this should be discussed thoroughly with your healthcare provider as pills come with their own set of risks.
5. Avoid hormone replacement therapy (HRT): If you’re going through menopause, avoid or limit hormone therapy. If you need to take it, use the lowest dose for the shortest time.
6. Regular check-ups: Make sure you have regular pelvic examinations, Pap tests, and human papillomavirus (HPV) vaccinations. Early detection of pre-cancerous conditions can help in preventing uterus cancer.
7. Treat underlying health conditions: Conditions like Polycystic Ovary Syndrome (PCOS), diabetes, or any condition that can alter hormone levels in your body could potentially increase your risk for uterine cancer. Treating these conditions and keeping them under control can help prevent the development of uterine cancer.
Always remember, these are preventive measures, and they reduce the risk but do not completely eliminate the chance of getting uterus cancer. It’s also important to consult with your doctor about your risk of womb cancer and the best methods to prevent it.
FAQ’s about Womb (uterus) cancer
1. What is womb (uterus) cancer?
Womb cancer, or uterine cancer, is a common type of cancer that affects the uterus. The most common type is endometrial cancer, which starts in the lining of the womb.
2. What are the symptoms of womb (uterus) cancer?
The most common symptom is abnormal vaginal bleeding, such as heavier or irregular periods, spotting between periods, or bleeding after menopause. Other possible symptoms can include pain during sex, pelvic pain and unusual vaginal discharge.
3. What causes womb (uterus) cancer?
While the exact cause is not known, womb cancer is often linked with changes in hormone levels, particularly an increase in estrogen. Risk factors can include age, family history, obesity, and use of hormone therapy after menopause.
4. How is womb (uterus) cancer diagnosed?
Womb cancer is often detected during routine pelvic exams, or can be diagnosed after investigating the cause of abnormal bleeding. A biopsy, or sample of tissue, can be taken from the uterus and tested for cancer cells. Imaging tests, such as ultrasounds, CT scans or MRI scans can also be used.
5. How is womb (uterus) cancer treated?
Treatment for womb cancer depends on the individual and the stage of the disease. Options can include surgery to remove the uterus (hysterectomy), radiation therapy, chemotherapy, hormone therapy or a combination of these approaches.
6. Is womb (uterus) cancer curable?
Womb cancer is often curable if detected in the early stages. The prognosis can depend on factors such as the type and stage of the cancer, and the overall health of the patient.
7. What is the survival rate for womb (uterus) cancer?
Survival rates can vary widely based on factors like cancer stage, patient age and overall health. However, in general, the 5-year survival rate for women with localized endometrial cancer is around 95% according to The American Cancer Society.
8. How can I reduce my risk of developing womb (uterus) cancer?
Having regular pelvic exams, maintaining a healthy weight, and treating conditions like polycystic ovary syndrome (which can increase estrogen levels) can lower your risk. Long-term use of oral contraceptives and staying physically active can also help reduce your risk.
Always consult with your doctor or a healthcare professional for medical advice and regular check-ups to ensure early detection.
Useful links
Womb (uterus) cancer, also known as Endometrial cancer, is a common type of cancer that begins in the layer of cells that form the lining (endometrium) of the uterus. Here are a few high level journals with links that provide detailed information about Womb (uterus) cancer.
Always consult with healthcare professionals for accurate information. Reading materials from journals can help you understand the condition and its management strategies better but should not be considered as a form of treatment advice.
Complications of Womb (uterus) cancer
Uterine cancer, also known as womb cancer, can have several complications depending on various factors such as the stage of the cancer, overall health of the patient, and the plan and outcomes of treatment. Here are some potential complications:
1. Spread of Cancer (Metastasis): In advanced stages, cancer can spread from the uterus to other parts of the body including the bladder, rectum, lungs, liver, or even the bones. This can lead to a variety of health issues depending on where the cancer has spread.
2. Recurrence: Even after successful treatment, there is always a risk that the cancer may return. Regular post-treatment checkups are vital to monitor for recurrence.
3. Side Effects of Treatment: Treatments for uterine cancer, including surgery, chemotherapy, and radiation therapy, have potential side effects. Surgery may result in pain and a lengthy recovery period. Chemotherapy and radiation therapy can cause fatigue, hair loss, nausea, loss of appetite, and other uncomfortable side effects.
4. Emotional Issues: The diagnosis and treatment of uterine cancer can lead to a significant amount of stress, anxiety, and depression. The disease and its treatment can also impact body image and self-esteem, which may lead to emotional and psychological issues.
5. Fertility Issues: Treatment for uterine cancer, particularly in younger women, can have a significant impact on fertility. Certain treatments might necessitate the removal of the uterus (hysterectomy), thus making natural conception impossible.
6. Long-Term Health Issues: Survivors of uterine cancer may face long-term health issues, including lymphedema (swelling caused by a blockage in the lymphatic system, primarily in the legs), sexual problems, early menopause, bowel and bladder problems, and an increased risk of other cancers.
The exact complications that one may experience can vary greatly from person to person, and it’s always best to discuss with the health care team managing the cancer for exact details and potential treatments or management strategies.
Home remedies of Womb (uterus) cancer
Uterine cancer is a serious condition that needs professional medical treatment, which may involve surgery, radiation therapy, chemotherapy, or targeted therapy.
However, certain practices could complement your doctor-prescribed treatment plan, help to manage symptoms, boost health and enhance quality of life. These include:
1. Proper Nutrition: Eating a healthy diet full of fresh fruits, vegetables, and whole grains can help ensure your body gets all the nutrients it needs. A balanced diet can help you maintain physical strength and speed up recovery.
2. Physical Activity: Light exercises within your comfort level, like walking, can help to enhance physical strength and reduce fatigue levels. Always consult your doctor before starting any exercise routine.
3. Regular Monitoring: Keep regular follow-ups with your doctor for tracking progress.
4. Mental and Emotional care: Activities such as meditation, yoga, counseling, or support groups might help in managing stress and maintaining emotional balance.
5. Adequate Rest: Adequate rest and good sleep are critical to help your body recover.
6. Hydration: Drinking plenty of water can help your body process chemotherapy drugs and reduce the risk of constipation.
Remember, these practices can help to support overall health and quality of life during cancer treatment, but they aren’t substitutes for medical treatments. Consult your healthcare provider before starting any practices.
Lastly, early detection is key in managing various cancers, including uterine cancer. Regular screenings, routine gynecologic examinations, and awareness of symptoms (like abnormal vaginal bleeding) significantly increase the chances of early diagnosis and successful treatment.